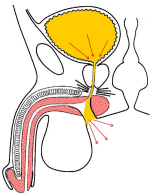
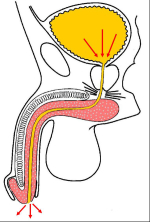
| “会阴尿道造口术”是在会阴部肛门上方进行造口(图1),避免尿液通过原尿道全长(图2)。在接受手术以后,男性尿道由原来的长12-18cm缩短为接近女性尿道的长度,大约5-6cm,使得尿液更加容易排出。 | |
|
图 1 |
图 2 |
| 会阴尿道造口不会造成尿失禁,也不需要使用尿垫和尿管。患者须行坐位排尿,并非以原龟头的尿道口排尿。会阴造口位置隐蔽(图3,4),在站立位时不易被发现。 | |
|
图 3 |
图 4 |
会阴部尿道造口术一般适用于以下人群:
- 患有浅表膀胱肿瘤造成尿道狭窄的患者,需进行反复膀胱镜检查或内镜下肿瘤切除。通过会阴尿道造口,泌尿外科医生可以进行膀胱镜检查,患者也几乎不承受任何痛苦。
- 有神经源性膀胱,膀胱憩室,残尿量高的患者。在此手术后可以使尿道长度更短,利于排空膀胱。
- 对于先前接受过多次手术治疗尿道狭窄失败的,再次手术复发率高。
- 全身状况较差的高龄患者,不能耐受长时间麻醉的。
讲座 1:
| Uretroplastia en dos tiempos ¿cómo y cuándo ? 51 Curso de Urologia Fundació Puigevert 18 – 20 de octubre 2006 Barcelona – Spain |
 download PDF |
论文 1
Peterson AC, Palminteri E, Lazzeri M, Guanzoni G, Barbagli G, Webster GD.
Heroic measures may not always be justified in extensive urethral stricture due to lichen sclerosus (balanitis xerotica obliterans).
Urology. 2004 Sep;64(3):565-8.
论文 2
Peterson AC, Palminteri E, Lazzeri M, Guanzoni G, Barbagli G, Webster GD.
Heroic measures may not always be justified in extensive urethral stricture due to lichen sclerosus (balanitis xerotica obliterans).
Urology. 2004 Sep;64(3):565-8.
论文 2
Guido Barbagli, Michele De Angelis, Giuseppe Romano and Massimo Lazzeri
Clinical outcome and quality of life assessment in patients treated with perineal urethrostomy for anterior urethral stricture disease
J Urol, 2009: 182, 548-557
1. 问: 此项手术使用什么麻醉方式?
答: 经口气管插管的全身麻醉。
2. 问: 手术时间多长?
答: 约2小时。
3. 问: 手术后是否有勃起、生育问题或者尿失禁的风险?
答: 没有。
4. 问: 手术后住院时间是多长?
答: 一般来讲,5到7天
5. 问: 术后多长时间可以拔除尿管?
答: 至少保留至术后2周。
6. 问: 恢复期有什么特别需要注意的问题么?
答: 在恢复期,抗生素的使用一般持续到尿管拔除以后。同时,长途坐车旅行,重体力劳动、性生活以及运动是暂时需要避免的。
7. 问: 术后什么时候可以恢复工作、性生活以及运动?
答: 在拔除尿管的一个月后,根据情况逐步恢复即可。
8. 问: 手术以后是否可以立即骑自行车或摩托车?
答: 不建议术后立即进行骑车、骑马等运动。
9. 问: 术后饮食需要注意些什么?
答: 避免啤酒以及烈性酒精饮品,巧克力,可可,坚果和贝类不要多吃。
答: 经口气管插管的全身麻醉。
2. 问: 手术时间多长?
答: 约2小时。
3. 问: 手术后是否有勃起、生育问题或者尿失禁的风险?
答: 没有。
4. 问: 手术后住院时间是多长?
答: 一般来讲,5到7天
5. 问: 术后多长时间可以拔除尿管?
答: 至少保留至术后2周。
6. 问: 恢复期有什么特别需要注意的问题么?
答: 在恢复期,抗生素的使用一般持续到尿管拔除以后。同时,长途坐车旅行,重体力劳动、性生活以及运动是暂时需要避免的。
7. 问: 术后什么时候可以恢复工作、性生活以及运动?
答: 在拔除尿管的一个月后,根据情况逐步恢复即可。
8. 问: 手术以后是否可以立即骑自行车或摩托车?
答: 不建议术后立即进行骑车、骑马等运动。
9. 问: 术后饮食需要注意些什么?
答: 避免啤酒以及烈性酒精饮品,巧克力,可可,坚果和贝类不要多吃。
| 更新至2021年12月31日 | |||

PDF |
|||
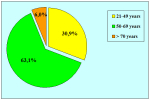
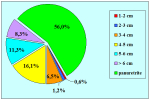
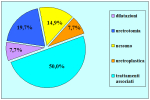
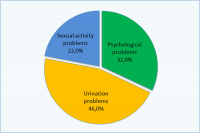
患者会阴尿道造口术后生活质量调查
173位患者参与调查
Barbagli G. 等, J Urol 2009: 182, 548 – 557
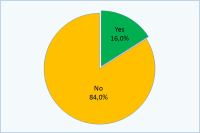
会阴尿道造口术是否给您造成了任何的困扰?
| 是:16% 不是:84% |
如果回答:是:
| 心理性的 32% 排尿困难: 46% 性生活问题 : 22% |
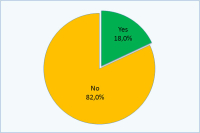
您与伴侣是否在术后性生活不愉快?
| 是: 18% 不是:82% |
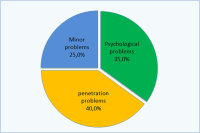
如果回答:是:
| 心里性的:35% 插入困难:40% 小问题:25% |
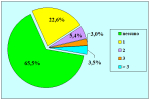
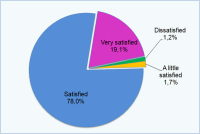
您对手术效果是否满意?
| 不满意:1.2% 还可以:1.7% 满意:78% 非常满意:19.1% |
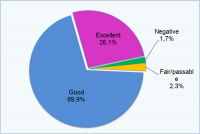
您怎样评价目前生活?
| 不好:1.7% 凑合:2.3% 不错:69.9% 非常好:26.1% |
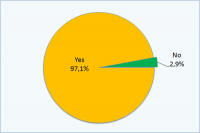
您会再次接受本手术么?
| 是:97.1% 不会:2.9% |
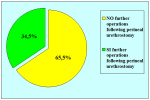
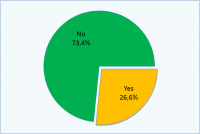
您是否希望通过二次手术恢复自然状态排尿?
| 是: 26.6% 否:73.4% |
操作详解
 download PDF |