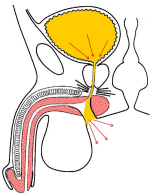
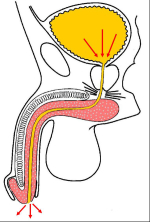
| The surgical technique of “Perineal urethrostomy” is to create a new urethral opening via the perineum, just above the anus (figure 1), thus avoiding that urine need to travel through the entire length of the urethra (figure 2). Using this technique the male urethra, 12-18 cm long, becomes similar to the female urethra, 5-6 cm long. This change permits that the bladder requires a shorter tract to push out urine. | |
|
figure 1 |
figure 2 |
| The surgical technique of Perineal urethrostomy does not interfere with urinary continence and does not require the use of external pads or catheter. The patient is requested to void in a seated position because urinary flow is through the perineal opening and no longer through the apex of the glans. This perineal opening is concealed (figures 3 – 4) and is not visible when the patient is in a standing position. | |
|
figure 3 |
figure 4 |
The surgical technique of Perineal urethrostomy is basically suggested in the following cases:
- Patients with urethral strictures associated with superficial bladder tumor which requires periodical cystoscopy or endoscopic removal of the tumor. By using the perineal opening, it is easy for the urologist to perform any endoscopic procedure. For the patient, this procedure is painless.
- Patients with urethral strictures associated with neurogenic bladder, bladder diverticula, showing high post-voiding residual urine volume. Since the urethra is shorter after the procedure, it is easier to obtain a complete emptying of the bladder.
- Patients with urethral strictures who had undergone previous and numerous failed surgical attempts to repair urethral stricture disease, showing a high risk of stricture recurrence rate.
- Elderly patients with urethral strictures associated with poor general health conditions in which an extended time under anesthesia in order to perform complex urethral repair is not suggested.
| Uretroplastia en dos tiempos ¿cómo y cuándo ? 51 Curso de Urologia Fundació Puigevert 18 – 20 de octubre 2006 Barcelona – Spain |
 download PDF |
Article n° 1
Peterson AC, Palminteri E, Lazzeri M, Guanzoni G, Barbagli G, Webster GD.
Heroic measures may not always be justified in extensive urethral stricture due to lichen sclerosus (balanitis xerotica obliterans).
Urology. 2004 Sep;64(3):565-8.
Article n° 2
Guido Barbagli, Michele De Angelis, Giuseppe Romano and Massimo Lazzeri
Clinical outcome and quality of life assessment in patients treated with perineal urethrostomy for anterior urethral stricture disease
J Urol, 2009: 182, 548-557
Answer: General anesthesia with oro-tracheal intubation.
2. Question: How many hours does the surgery take?
Answer: About 2 hours.
3. Question: Are there any risks concerning erection, fertility and urinary incontinence after the surgery?
Answer: No, there aren’t.
4. Question: How many days of hospital recovery are expected following the surgery?
Answer: In general, from 5 to 7 days.
5. Question: How long will I have to use a catheter after the surgery?
Answer: The urethral catheter must stay in place for two weeks after the surgery.
6. Question: Are there any particular recommendations during convalescence?
Answer: During convalescence, the use antibiotics until the catheter is removed is suggested. Avoiding long car trips, as well as heavy labor and sexual and sports activities are also suggested.
7. Question: When will I be able to resume my working, sexual and sports activities?
Answer: All these activities can be gradually resumed about 30 days after the removal of the catheter.
8. Question: Can I ride a bike or a motorcycle immediately after the surgery?
Answer: It is not recommended to ride bikes, motorcycles or horses after the surgery.
9. Question: What kinds of foods and drinks should be avoided after the surgery?
Answer: Beer and sparkling wines should be avoided, as well as large quantities of chocolate, cocoa, nuts and shellfish.
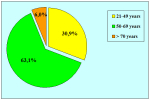
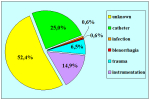
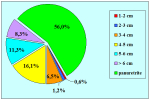
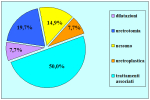
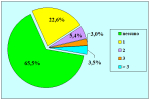
| Up-to-date to 12-31-2021 | |||

Summarizing table |
|||
QUESTIONNAIRE ON PATIENT QUALITY OF LIFE AFTER PERINEAL URETHROSTOMY
Results on 173 patients
Barbagli G. et al, J Urol 2009: 182, 548 – 557
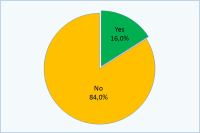
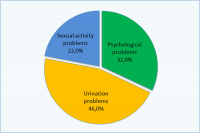
Has the perineal urethrostomy caused you any problems?
| Yes 16% No 84% |
If you answered Yes:
| Psychological problems 32% Urination problems 46% Sexual activity problems 22% |
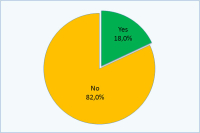
Have you had problems with your partner due to this operation?
| Yes 18% No 82% |
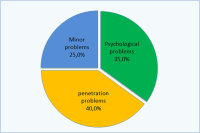
If you answered Yes:
| Psychological problems 35% Penetration problems 40% Minor problems 25% |
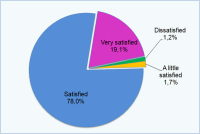
Are you pleased with the results obtained with surgery?
| Dissatisfied 1.2% A little satisfied 1.7% Satisfied 78% Very satisfied 19.1% |
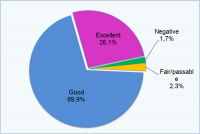
How would you evaluate these results?
| Negative 1.7% Fair/passable 2.3% Good 69.9% Excellent 26.1% |
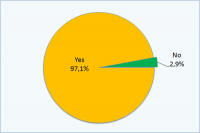
Would you undergo this type of operation again?
| Yes 97.1% No 2.9% |
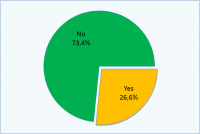
Would you like to undergo second stage urethroplasty to restore normal urinary function?
| Yes 26.6% No 73.4% |
Surgical Technique: step by step
 download PDF |