“口腔黏膜获取术”是从口腔中取一块黏膜组织的手术。
分为两种类型:
分为两种类型:
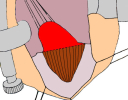
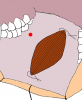
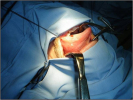
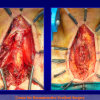
- 从颊粘膜获取黏膜移植物。这种技术是从口腔颊部的黏膜获取移植物(如图1,2,3,4),在本中心使用最为广泛。
- 从舌获取黏膜移植物。这种技术是从舌体的腹侧获取黏膜移植物(如图5,6,7,8,9)。这种技术一般在颊粘膜无法获取的情况下使用。
口腔黏膜获取术一般是在有如下情况时使用:
- 患者存在尿道球部或是阴茎部的狭窄,在进行扩大尿道成形术时需要自体材料。
一些患者可能需要从口腔取两处移植物(图10)。口腔取移植物的操作几乎没有并发症,并且根据我们对350位患者的问卷调查来看,患者的满意程度以及对操作的接受程度也很高(见调查问卷)。
|
图 1 |
图 2 |
图 3 |
图 4 |
图 5 |
|
图 6 |
图 7 |
图 8 |
图 9 |
图 10 |
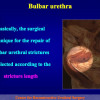
讲座 1:
| Urethral stricture surgery – tips and tricks. Surgery of the bulbar urethra Joint Meeting of the ESAU and the ESGURS October 25 – 27, 2007 Madrid – Spain |
 Download PDF Download PDF |
|
|
|
||
|
讲座 2: Evaluation of early, late complications and patient satisfaction in 300 patients who underwent oral graft harvesting from a single cheek using a standard technique in a referral center experience AUA 2009 Chicago, Illinois – USA April 25 – 30, 2009 |
 Download PDF Download PDF |
|
|
|
||
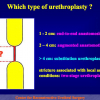
| 讲座 3: One-stage substitution urethroplasty 24th Annual EAU Congress Stockholm – Sweden March 17 – 21, 2009 |
 Download PDF Download PDF |
|
|
|
||
| 讲座 4: The Use of Oral Mucosa for Anterior Urethroplasty Training Course on “Techniques in Reconstructive Urology” Mansoura – Egypy January 23 – 29, 2010 |
 Download PDF Download PDF |
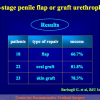
论文 1
Guido Barbagli, Michele De Angelis, Giuseppe Romano, Pier Guido Ciabatti, Massimo Lazzeri,
The Use of Lingual Mucosal Graft in Adult Anterior Urethroplasty: Surgical Steps and Short-Term Outcome
Eur Urol 2008; 54:671 – 676
论文° 2
Lu-Jie Song; Yue-Min Xu; Massimo Lazzeri; Guido Barbagli
Lingual mucosal grafts for anterior urethroplasty: a review
BJU International, 2009: 104, 1052-1056
论文 3
Barbagli G, Vallasciani S, Romano G, Fabbri F, Guazzoni G, Lazzeri M.
Morbidity of Oral Mucosa Graft Harvesting from a Single Cheek
Eur Urol, 2010: 58, 33 – 41
论文 4
Guido Barbagli , Salvatore Sansalone , Giuseppe Romano and Massimo Lazzeri
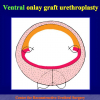
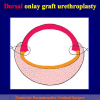
Ventral onlay oral mucosal graft bulbar urethroplasty
BJU Int 2011; 108: 1218-1231
论文 5
Guido Barbagli, Salvatore Sansalone, Massimo Lazzeri
Oral Mucosa and Urethroplasty: It’s Time to Change
EUROPEAN UROLOGY 6 2 ( 2 0 1 2 ) 1 0 7 1 – 1 0 7 5
Guido Barbagli, Michele De Angelis, Giuseppe Romano, Pier Guido Ciabatti, Massimo Lazzeri,
The Use of Lingual Mucosal Graft in Adult Anterior Urethroplasty: Surgical Steps and Short-Term Outcome
Eur Urol 2008; 54:671 – 676
论文° 2
Lu-Jie Song; Yue-Min Xu; Massimo Lazzeri; Guido Barbagli
Lingual mucosal grafts for anterior urethroplasty: a review
BJU International, 2009: 104, 1052-1056
论文 3
Barbagli G, Vallasciani S, Romano G, Fabbri F, Guazzoni G, Lazzeri M.
Morbidity of Oral Mucosa Graft Harvesting from a Single Cheek
Eur Urol, 2010: 58, 33 – 41
论文 4
Guido Barbagli , Salvatore Sansalone , Giuseppe Romano and Massimo Lazzeri
Ventral onlay oral mucosal graft bulbar urethroplasty
BJU Int 2011; 108: 1218-1231
论文 5
Guido Barbagli, Salvatore Sansalone, Massimo Lazzeri
Oral Mucosa and Urethroplasty: It’s Time to Change
EUROPEAN UROLOGY 6 2 ( 2 0 1 2 ) 1 0 7 1 – 1 0 7 5
1. 问题:: 问:手术费是否可以由国家保健系统(意大利)全额负担?
回答: 是的。
2. 问题:: 此项手术使用什么麻醉方式?
回答: 经鼻插管的全身麻醉。
3. 问题:: 手术时间多长?
回答: 颊粘膜取移植物手术大约半小时。
4. 问题:: 手术后是否有咀嚼功能障碍、流涎问题或者容貌改变的风险?
回答: 没有。
5. 问题: 手术后住院时间是多长?
回答: 口腔黏膜尿道成形术一般5到7天
6. 问题:从口腔取移植物术后是否很痛?
回答: 不痛。仅仅3.7%的患者需要解热镇痛药物来消除口腔的疼痛感。
7. 问题: 术后多长时间才能恢复正常饮食?
回答: 患者一般首先进食纯流食和冰激凌,然后慢慢过度到软食和正常饮食。
8. 问题: 术后饮食需要注意些什么?
回答: 避免过热的食物。
9. 问题: 术后是否马上可以进行正常饮食?
回答: 所有患者都可以在术后一个月之内恢复到正常饮食。
10. 问题: 是否存在口干、张口困难、饭后肿胀或是不能微笑等风险?
回答: 没有。
回答: 是的。
2. 问题:: 此项手术使用什么麻醉方式?
回答: 经鼻插管的全身麻醉。
3. 问题:: 手术时间多长?
回答: 颊粘膜取移植物手术大约半小时。
4. 问题:: 手术后是否有咀嚼功能障碍、流涎问题或者容貌改变的风险?
回答: 没有。
5. 问题: 手术后住院时间是多长?
回答: 口腔黏膜尿道成形术一般5到7天
6. 问题:从口腔取移植物术后是否很痛?
回答: 不痛。仅仅3.7%的患者需要解热镇痛药物来消除口腔的疼痛感。
7. 问题: 术后多长时间才能恢复正常饮食?
回答: 患者一般首先进食纯流食和冰激凌,然后慢慢过度到软食和正常饮食。
8. 问题: 术后饮食需要注意些什么?
回答: 避免过热的食物。
9. 问题: 术后是否马上可以进行正常饮食?
回答: 所有患者都可以在术后一个月之内恢复到正常饮食。
10. 问题: 是否存在口干、张口困难、饭后肿胀或是不能微笑等风险?
回答: 没有。
“口腔黏膜获取术”问卷调查表
350位患者的调查结果
Barbagli G. et al, Eur Urol, 2010: 58,33 – 41
术后早期并发症
1. 是否有口腔黏膜取移植物手术后3天内出血情况?
| 是 4.3% 未出现 95.7% |
2. 对于口腔黏膜取移植物手术后的口腔疼痛如何评价?
| 不痛 49.2% 轻度疼痛 36% 中度疼痛 13.7% 非常痛 1.1% |
3. 口腔黏膜取移植物手术后3天口腔肿胀情况是怎样的?
| 无肿胀 33.7% 轻度肿胀 41.2% 中度肿胀 24.6% 重度肿胀 0.5% |
4. 术后多长时间开始正常饮食?
| 3天后 58.6% 6天后 31.4% 10天后 10% |
5. 在术后早期最困扰您的是什么?
| 口腔内的伤口 27.7% 会阴部的伤口 52.6% 两者都有 1.4% 都没有 18.3% |
6. 您是否在口腔黏膜取移植物手术后3天内服用止痛药?
| 是 3.7% 不是 96.3% |
术后晚期并发症
1. 术后多长时间口腔内的麻木感消失?
| 一周 73.4% 一个月 22.9% 3个月 2.7% |
2. 由于口腔内的缝合所致的口腔麻木您如何分级?
| 无麻木感 48% 轻度麻木 40.3% 中度麻木 10.9% 重度麻木 0.8% |
3. 由于口腔内的缝合所致的口腔麻木术后多长时间消失?
| 1个月 93.9% 2个月 4.4% 3个月 1.7% |
4. 由于口腔内的疤痕所致的口腔麻木如何分级?
| 无麻木感 82.8% 轻度麻木 14.6% 中度麻木 2.6% 重度麻木 0% |
5. 术后是否出现口腔感染情况?
| 有 1.7% 没有 98.3% |
6. 术后数月,您是否还有如下情况?
| 口腔内的感觉异常 2.3% 口腔麻木 10.3% 口腔疼痛 0% 没有不适感 87.4% |
7. 术后数月,您是否存在张口困难?
| 不是 98.3% 轻度 1.4% 中度 0.3% 重度 0% |
8. 术后数月,您是否存在不能微笑?
| 不存在 99.7% 轻度 0.3% 中度 0% 重度 0% |
9. 术后数月,您是否存在口干?
| 不存在 97.1% 轻度 2.6% 中度 0.3% 重度 0% |
10. 术后数月,您是否存在进食后口腔肿胀?
| 不存在 98.3% 轻度 1.7% 中度 0% 重度 0% |
11. 术后您最终是否恢复了正常饮食?
| 是 100% 否 0% |
12. 术后恢复饮食一般需要经过多长时间?
| 最多一个月 94% 2个月 4.3% 3个月 1.7% |
13. 您是否愿意再次接受此项手术?
| 是 98% 不愿意 2% |
 Download PDF |
Harvesting oral mucosal graft from the cheek:
|
 Download PDF |
Harvesting oral mucosal graft from the tongue:
|