There are two basic types of Harvesting oral mucosa from the mouth:
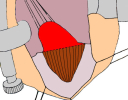
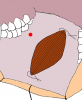
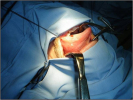
- Harvesting the oral mucosal graft from the cheek. Using this technique, the oral graft is harvested from the internal surface of the cheek (figures 1,2,3,4). This procedure is the most frequent technique used in our Center.
- Harvesting the oral mucosal graft from the tongue. Using this technique, the oral graft is harvested from the ventral surface of the tongue (figures 5,6,7,8,9). This procedure is used when the harvesting from the cheek is not possible.
The surgical technique of Harvesting oral mucosa from the mouth is generally suggested in the following case:
- patients with penile or bulbar urethral strictures, requiring an augmented urethroplasty using a substitute material.
In some patients may be necessary to harvest two grafts from the mouth (figure 10). The harvesting procedure of oral mucosa from the mouth is free of complications and the patient satisfaction and acceptance of this procedure is high, as we investigated using using a questionnaire in 350 patients. (see questionnaire)
|
Figure 1 |
Figure 2 |
Figure 3 |
Figure 4 |
Figure 5 |
|
Figure 6 |
Figure 7 |
Figure 8 |
Figure 9 |
Figure 10 |
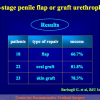
| Urethral stricture surgery – tips and tricks. Surgery of the bulbar urethra Joint Meeting of the ESAU and the ESGURS October 25 – 27, 2007 Madrid – Spain |
 Download PDF Download PDF |
|
|
|
||
|
Lecture n° 2: Evaluation of early, late complications and patient satisfaction in 300 patients who underwent oral graft harvesting from a single cheek using a standard technique in a referral center experience AUA 2009 Chicago, Illinois – USA April 25 – 30, 2009 |
 Download PDF Download PDF |
|
|
|
||
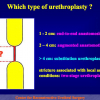
| Lecture n° 3: One-stage substitution urethroplasty 24th Annual EAU Congress Stockholm – Sweden March 17 – 21, 2009 |
 Download PDF Download PDF |
|
|
|
||
| Lecture n° 4: The Use of Oral Mucosa for Anterior Urethroplasty Training Course on “Techniques in Reconstructive Urology” Mansoura – Egypy January 23 – 29, 2010 |
 Download PDF Download PDF |
Guido Barbagli, Michele De Angelis, Giuseppe Romano, Pier Guido Ciabatti, Massimo Lazzeri,
The Use of Lingual Mucosal Graft in Adult Anterior Urethroplasty: Surgical Steps and Short-Term Outcome
Eur Urol 2008; 54:671 – 676
Article n° 2
Lu-Jie Song; Yue-Min Xu; Massimo Lazzeri; Guido Barbagli
Lingual mucosal grafts for anterior urethroplasty: a review
BJU International, 2009: 104, 1052-1056
Article n° 3
Barbagli G, Vallasciani S, Romano G, Fabbri F, Guazzoni G, Lazzeri M.
Morbidity of Oral Mucosa Graft Harvesting from a Single Cheek
Eur Urol, 2010: 58, 33 – 41
Article n° 4
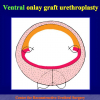
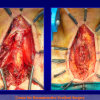
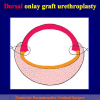
Guido Barbagli , Salvatore Sansalone , Giuseppe Romano and Massimo Lazzeri
Ventral onlay oral mucosal graft bulbar urethroplasty
BJU Int 2011; 108: 1218-1231
Article n° 5
Guido Barbagli, Salvatore Sansalone, Massimo Lazzeri
Oral Mucosa and Urethroplasty: It’s Time to Change
EUROPEAN UROLOGY 6 2 ( 2 0 1 2 ) 1 0 7 1 – 1 0 7 5
Answer: Yes.
2. Question: What kind of anesthesia is used for this surgery?
Answer: General anesthesia with nasal tube.
3. Question: How many hours does the surgery take?
Answer: Harvesting oral mucosa from the cheek takes about ½ hour.
4. Question: Are there any risks concerning chewing, flow of saliva and face physiognomy after the surgery?
Answer: No, there aren’t.
5. Question: How many days of hospital recovery are expected following the surgery?
Answer: Urethroplasty using oral mucosa requires from 5 to 7 days in hospital.
6. Question: Is it painful to harvest oral mucosa from the cheek?
Answer: No, it isn’t. Only 3.7% of patients required anti-inflammatory pain killers for oral pain.
7. Question: How many days shall I wait before resuming a normal diet?
Answer: The patient initially consumes a clear liquid diet and ice cream before advancing to a soft and then regular diet.
8. Question: Are there any food to avoid during the convalescence?
Answer: Very hot food.
9. Question: Can I resume eating normally after surgery?
Answer: All patients resumed eating normally after surgery within one month.
10. Question: Are there any risks such as dry mouth, difficulty at opening the mouth or swelling after eating, problems at smiling?
Answer: No, there aren’t.
QUESTIONNAIRE ON COMPLICATIONS FOLLOWING ORAL MUCOSA HARVESTING
Results on 350 patients
Barbagli G. et al, Eur Urol, 2010: 58,33 – 41
EARLY POST-OPERATIVE COMPLICATIONS
1. Did you suffer from bothersome bleeding during the three days following oral mucosa harvesting?
| Yes 4.3% No 95.7% |
2. How would you score the oral pain during the three days following oral mucosa harvesting?
| No pain 49.2% Slight 36% Moderate 13.7% Severe 1.1% |
3. How would you score the oral swelling during the three following oral mucosa harvesting?
| No swelling 33.7% Slight 41.2% Moderate 24.6% Severe 0.5% |
4. Following surgery, when did you resume a normal diet?
| After 3 days 58.6% After 6 days 31.4% After 10 days 10% |
5. What bothered you most during the early post-operative period?
| The oral wound 27.7% The perineal wound 52.6% Both 1.4% Neither 18.3% |
6. Did you take pain killers during the three days following oral mucosa harvesting?
| Yes 3.7% No 96.3% |
LATE POST-OPERATIVE COMPLICATIONS
1. How many days did oral numbness last after the surgery?
| 1 week 73.4% 1 month 22.9% 3 months 3.7% |
2. How would you rate the numbness experienced due to the oral stitches?
| No numbness 48% Slight 40.3% Moderate 10.9% Severe 0.8% |
3. Following surgery, how many months did the oral numbness last due to the stitches?
| 1 month 93.9% 2 months 4.4% 3 months 1.7% |
4. How would you score the numbness experienced due to the oral scar?
| No numbness 82.8% Slight 14.6% Moderate 2.6% Severe 0% |
5. Did you suffer from oral infection following the surgery?
| Yes 1.7% No 98.3% |
6. After some months following the surgery, do you have:
| Changes in oral sensitivity/sensibility/sensory perception 2.3% Oral numbness 10.3% Mouth pain 0% No problems 87.4% |
7. After some months following the surgery, do you have difficulties opening your mouth?
| No 98.3% Slight 1.4% Moderate 0.3% Severe 0% |
8. After some months following the surgery, do you have problems smiling?
| No 99.7% Slight 0.3% Moderate 0% Severe 0% |
9. After some months following the surgery, do you have dry mouth?
| No 97.1% Slight 2.6% Moderate 0.3% Severe 0% |
10. After some months following the surgery, do you have oral swelling after eating?
| No 98.3% Slight 1.7% Moderate 0% Severe 0% |
11. Did you resume eating normally following the surgery?
| Yes 100% No 0% |
12. How much time passed before resuming a normal diet?
| Up to 1 month 94% 2 months 4.3% 3 months 1.7% |
13. Would you undergo oral mucosa graft harvesting using this technique again?
| Yes 98% No 2% |
 Download PDF |
Harvesting oral mucosal graft from the cheek:
|
 Download PDF |
Harvesting oral mucosal graft from the tongue:
|