“皮肤或口腔黏膜移植尿道成形术”是在尿道狭窄处切开,以口腔黏膜移植物来增大尿道管径的手术。
|
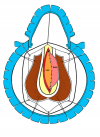
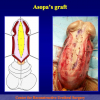
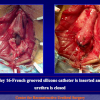
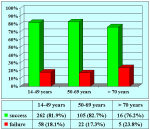
图 1 |
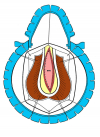
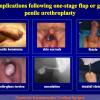
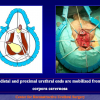
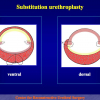
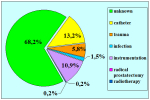
图 2 |
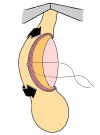
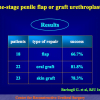
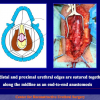
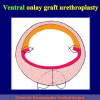
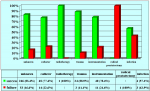
图 3 |
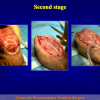
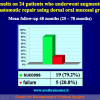
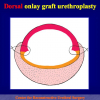
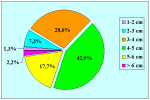
图 4 |
通常有四种方式:
- 腹侧口腔黏膜移植物尿道成形术。此术式中,移植物接合到尿道的腹侧(图1,2)。
- 背侧口腔黏膜移植物尿道成形术。此术式中,移植物接合到尿道的背侧(图3,4)。
- 侧向口腔黏膜移植物尿道成形术。此术式中,移植物接合到尿道的外侧。
- 完全口腔黏膜移植物尿道成形术。此术式中,移植物完全代替狭窄的尿道。
本术式适用于不存在损伤性尿道球部狭窄,且狭窄长度大于2cm。
讲座 1:
| Penile and bulbar urethroplasty Surgical techniques and results Hong Kong Urological Association Urethroplasty Workshop Division of Urology – Tuen Mun Hospital February 9 – 10, 2009 Hong Kong |
 Download PDF Download PDF |
论文 1
论文 2
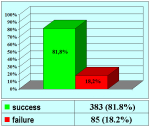
Barbagli G., Guazzoni G., Lazzeri M.
One-Stage bulbar urethroplasty: Retrospective analisys of the results in 375 patients
Eur Urol 2008; 53:828-33
论文 3
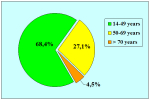
Guido Barbagli , Salvatore Sansalone , Giuseppe Romano and Massimo Lazzeri
Ventral onlay oral mucosal graft bulbar urethroplasty
BJU Int 2011; 108: 1218-1231
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Bulbar urethroplasty using buccal mucosa grafts placed on the ventral, dorsal or lateral surface of the urethra: are results affected by the surgical technique?
J Urol. 2005 Sep;174(3):955-7
论文 2
Barbagli G., Guazzoni G., Lazzeri M.
One-Stage bulbar urethroplasty: Retrospective analisys of the results in 375 patients
Eur Urol 2008; 53:828-33
论文 3
Guido Barbagli , Salvatore Sansalone , Giuseppe Romano and Massimo Lazzeri
Ventral onlay oral mucosal graft bulbar urethroplasty
BJU Int 2011; 108: 1218-1231
1. 问: 此项手术使用什么麻醉方式?
答: 经鼻的全身麻醉。
2. 问: 手术时间多长?
答: 约2小时。
3. 问: 手术后是否有勃起、生育问题或者尿失禁的风险?
答: 没有。
4. 问: 手术后住院时间是多长?
答: 一般来讲,5到7天
5. 问: 术后多长时间可以拔除尿管?
答: 至少保留至术后4周,待术后首次尿路造影结果正常后拔除。
6. 问: 恢复期有什么特别需要注意的问题么?
答: 在恢复期,抗生素的使用一般持续到尿管拔除以后。同时,长途坐车旅行,重体力劳动、性生活以及运动是暂时需要避免的。
7. 问: 术后什么时候可以恢复工作、性生活以及运动?
答: 在拔除尿管的一个月后,根据情况逐步恢复即可。
8. 问: 手术以后是否可以立即骑自行车或摩托车?
答: 不建议术后立即进行骑车、骑马等运动。
9. 问: 术后饮食需要注意些什么?
答: 避免啤酒以及烈性酒精饮品,巧克力,可可,坚果和贝类不要多吃。
答: 经鼻的全身麻醉。
2. 问: 手术时间多长?
答: 约2小时。
3. 问: 手术后是否有勃起、生育问题或者尿失禁的风险?
答: 没有。
4. 问: 手术后住院时间是多长?
答: 一般来讲,5到7天
5. 问: 术后多长时间可以拔除尿管?
答: 至少保留至术后4周,待术后首次尿路造影结果正常后拔除。
6. 问: 恢复期有什么特别需要注意的问题么?
答: 在恢复期,抗生素的使用一般持续到尿管拔除以后。同时,长途坐车旅行,重体力劳动、性生活以及运动是暂时需要避免的。
7. 问: 术后什么时候可以恢复工作、性生活以及运动?
答: 在拔除尿管的一个月后,根据情况逐步恢复即可。
8. 问: 手术以后是否可以立即骑自行车或摩托车?
答: 不建议术后立即进行骑车、骑马等运动。
9. 问: 术后饮食需要注意些什么?
答: 避免啤酒以及烈性酒精饮品,巧克力,可可,坚果和贝类不要多吃。
| 更新至2021年12月31日 | |||

总结表 |
|||
操作详解
 Downloads PDF |