The surgical technique of “Urethroplasty with skin or oral mucosal graft” is made by opening the urethra at the level of the stricture site and widening the urethral lumen by applying an oral graft.
|
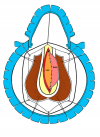
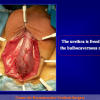
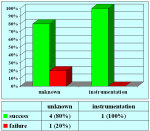
Figure 1 |
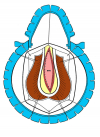
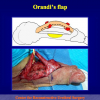
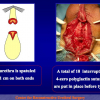
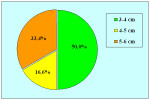
Figure 2 |
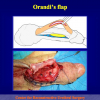
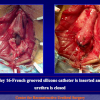
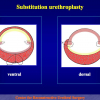
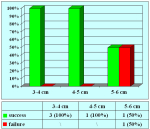
Figure 3 |
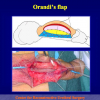
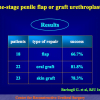
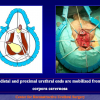
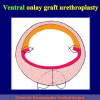
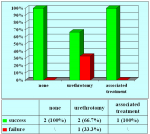
Figure 4 |
There are four basic types of Urethroplasty with skin or oral mucosal graft:
- Urethroplasty with ventral oral mucosal graft. Using this technique, the oral graft is sutured on the ventral site of the urethra (figures 1,2).
- Urethroplasty with dorsal skin or oral mucosal graft. Using this technique, the oral graft is sutured on the dorsal site of the urethra (figures 3,4).
- Urethroplasty with lateral oral mucosal graft. Using this technique, the oral graft is sutured on the lateral site of the urethra.
- Urethroplasty with complete substitution by oral mucosal graft. Using this technique, the urethral mucosa is completely replaced by an oral graft.
The surgical technique of Urethroplasty with skin or oral mucosal graft is generally suggested in the patients with no traumatic bulbar urethral strictures, more than 2 cm in length.
Lecture n° 1:
| Penile and bulbar urethroplasty Surgical techniques and results Hong Kong Urological Association Urethroplasty Workshop Division of Urology – Tuen Mun Hospital February 9 – 10, 2009 Hong Kong |
 scarica PDF |
Article n° 1
Article n° 2
Barbagli G., Guazzoni G., Lazzeri M.
One-Stage bulbar urethroplasty: Retrospective analisys of the results in 375 patients
Eur Urol 2008; 53:828-33
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Bulbar urethroplasty using buccal mucosa grafts placed on the ventral, dorsal or lateral surface of the urethra: are results affected by the surgical technique?
J Urol. 2005 Sep;174(3):955-7
Article n° 2
Barbagli G., Guazzoni G., Lazzeri M.
One-Stage bulbar urethroplasty: Retrospective analisys of the results in 375 patients
Eur Urol 2008; 53:828-33
1. Question: Can the surgical procedure be performed with full coverage by the National Health Care System?
Answer: Yes.
2. Question: What kind of anesthesia is used for this surgery?
Answer: General anesthesia with nasal intubation.
3. Question: How many hours does the surgery take?
Answer: About 2 hours.
4. Question: Are there any risks concerning erection, fertility and urinary incontinence after the surgery?
Answer: No, there aren’t.
5. Question: How many days of hospital recovery are expected following the surgery?
Answer: In general, from 5 to 7 days.
6. Question: How long will I have to use a catheter after the surgery?
Answer: The urethral catheter must stay in place for four weeks after the surgery, when the first post-operative voiding urethrography is done.
7. Question: Are there any particular recommendations during convalescence?
Answer: During convalescence, the use antibiotics until the catheter is removed is suggested. Avoiding long car trips, as well as heavy labor and sexual and sports activities are also suggested.
8. Question: When will I be able to resume my working, sexual and sports activities?
Answer: All these activities can be gradually resumed about 30 days after the removal of the catheter.
9. Question: Can I ride a bike or a motorcycle immediately after the surgery?
Answer: It is not recommended to ride bikes, motorcycles or horses after the surgery.
10. Question: What kinds of foods and drinks should be avoided after the surgery?
Answer: Beer and sparkling wines should be avoided, as well as large quantities of chocolate, cocoa, nuts and shellfish.
Answer: Yes.
2. Question: What kind of anesthesia is used for this surgery?
Answer: General anesthesia with nasal intubation.
3. Question: How many hours does the surgery take?
Answer: About 2 hours.
4. Question: Are there any risks concerning erection, fertility and urinary incontinence after the surgery?
Answer: No, there aren’t.
5. Question: How many days of hospital recovery are expected following the surgery?
Answer: In general, from 5 to 7 days.
6. Question: How long will I have to use a catheter after the surgery?
Answer: The urethral catheter must stay in place for four weeks after the surgery, when the first post-operative voiding urethrography is done.
7. Question: Are there any particular recommendations during convalescence?
Answer: During convalescence, the use antibiotics until the catheter is removed is suggested. Avoiding long car trips, as well as heavy labor and sexual and sports activities are also suggested.
8. Question: When will I be able to resume my working, sexual and sports activities?
Answer: All these activities can be gradually resumed about 30 days after the removal of the catheter.
9. Question: Can I ride a bike or a motorcycle immediately after the surgery?
Answer: It is not recommended to ride bikes, motorcycles or horses after the surgery.
10. Question: What kinds of foods and drinks should be avoided after the surgery?
Answer: Beer and sparkling wines should be avoided, as well as large quantities of chocolate, cocoa, nuts and shellfish.
| Up-to-date to 12-31-2013 | |||

Summarizing table |
|||