L’intervento denominato
“anastomosi termino-terminale” consiste nel sezionare completamente l’uretra nel punto in cui è presente la stenosi, asportare il tessuto cicatriziale e suturare insieme i due monconi ripristinando la continuità del canale. Questo intervento è uno di primi interventi descritti per la riparazione delle stenosi uretrali.
|
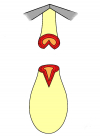
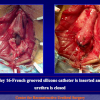
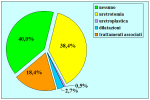
Figura 1
|
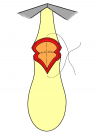
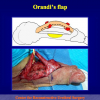
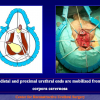
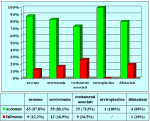
Figura 2
|
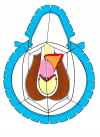
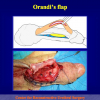
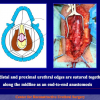
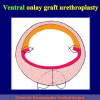
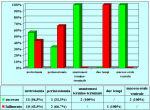
Figura 3
|
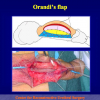
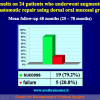
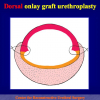
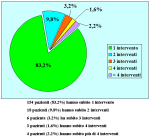
Figura 4
|
Fondamentalmente, esistono due tipi di anastomosi termino-terminale:
- Anastomosi termino-terminale. In questa procedura il canale uretrale viene completamente sezionato a livello della stenosi, il tessuto cicatriziale viene rimosso ed i due monconi uretrali vengono riavvicinati e suturati insieme (figure 1,2).
- Anastomosi termino-terminale con innesto di cute o mucosa orale. In questa procedura il canale uretrale viene completamente sezionato a livello della stenosi, il tessuto cicatriziale viene rimosso ed i due monconi uretrali vengono riavvicinati e suturati sopra un innesto di cute o mucosa orale (figure 3,4).
L’intervento chirurgico denominato anastomosi termino-terminale è indicato fondamentalmente nei seguenti casi:
- pazienti con stenosi traumatica dell’uretra bulbare, di lunghezza non superiore a 2 cm.
- pazienti già sottoposti, con esito negativo, ad intervento di uretroplastica che presentano una stenosi recidiva fibrosa ma non superiore a 2 cm di lunghezza.
Lettura n° 1:
Penile and bulbar urethroplasty Surgical techniques and results
Hong Kong Urological Association Urethroplasty Workshop Division of Urology – Tuen Mun Hospital
February 9 – 10, 2009
Hong Kong |
|

scarica PDF |
Articolo n° 1
Barbagli G, Palminteri E, Bartoletti R, Selli C, Rizzo M.
Long-term results of anterior and posterior urethroplasty with actuarial evaluation of the success rates.
J Urol. 1997 Oct;158(4):1380-2.
Purpose: We analyzed the long-term results of different urethroplasty techniques.
Materials and Methods: We performed a retrospective review of 98 patients who underwent different procedures for anterior (78) and posterior (20) urethral strictures. Mean followup was 53 months. A total of 20 patients underwent end-to-end anastomosis (group 1), 30 underwent 1-stage procedures (group 2), 28 underwent 2-stage procedures (group 3), and 20 underwent bulboprostatic anastomosis (group 4). The results were analyzed using Kaplan-Meier curves and log rank test.
Results: The success rate was 95% for group 1, 93.4% for group 2, 78.6% for group 3, and 70% for group 4. Statistical evaluation of the actuarial success rates failed to show significant differences among the 4 groups.
Conclusions: The stricture recurrences were uniformly distributed over time. Urethroplasty patients must be followed for the rest of their lives.
Articolo n° 2
Barbagli G, Palminteri E, Lazzeri M, Guazzoni G, Turini D.
Long-term outcome of urethroplasty after failed urethrotomy versus primary repair.
J Urol. 2001 Jun;165(6 Pt 1):1918-9.
Purpose: A urethral stricture recurring after repeat urethrotomy challenges even a skilled urologist. To address the question of whether to repeat urethrotomy or perform open reconstructive surgery, we retrospectively review a series of 93 patients comparing those who underwent primary repair versus those who had undergone urethrotomy and underwent secondary treatment.
Materials and Methods: From 1975 to 1998, 93 males between age 13 and 78 years (mean 39) underwent surgical treatment for bulbar urethral stricture. In 46 (49%) of the patients urethroplasty was performed as primary repair, and in 47 (51%) after previously failed urethrotomy. The strictures were localized in the bulbous urethra without involvement of penile or membranous tracts. The etiology was ischemic in 37 patients, traumatic in 23, unknown in 17 and inflammatory in 16. To simplify evaluation of the results, the clinical outcome was considered either a success or a failure at the time any postoperative procedure was needed, including dilation.
Results: In our 93 patients primary urethroplasty had a final success rate of 85%, and after failed urethrotomy 87%. Previously failed urethrotomy did not influence the long-term outcome of urethroplasty. The long-term results of different urethroplasty techniques had a final success rate ranging from 77% to 96%.
Conclusions: We conclude that failed urethrotomy does not condition the long-term result of surgical repair. With extended followup, the success rate of urethroplasty decreases with time but it is in fact still higher than that of urethrotomy.
Articolo n° 3
Guido Barbagli, Michele De Angelis, Giuseppe Romano and Massimo Lazzeri
Long-Term Followup of Bulbar End-to-End Anastomosis: A Retrospective Analysis of 153 Patients in a Single Center Experience
J Urol 2007; 178: 2470-2473
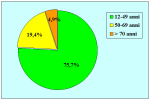
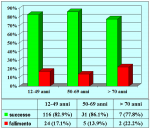
Purpose: We performed a retrospective evaluation and statistical analysis of outcome in patients who underwent bulbar end-to-end anastomosis.
Materials and Methods: We reviewed 153 patients with an average age of 39 years who underwent bulbar end-to-end anastomosis between 1988 and 2006. Mean followup was 68 months. Stricture etiology was unknown (62.7%), catheter (14.4%), blunt perineal trauma (11.7%), instrumentation (9.8%), radiotherapy (0.7%) and infection (0.7%). Stricture length was 1 to 2 cm (in 59.5%), 2 to 3 cm (37.9%), 3 to 4 cm (1.9%) or 4 to 5 cm (0.7%). A total of 90 patients (59%) underwent dilation, internal urethrotomy, urethroplasty or multiple procedures before being referred to our center. Clinical outcome was considered a treatment failure when any postoperative instrumentation was needed. The prevalence of postoperative sexual dysfunction was investigated using a nonvalidated questionnaire.
Results: Of 153 cases 139 (90.8%) were successful and 14 (9.2%) were treatment failures. Treatment failure was managed with urethrotomy in 9 cases, end-to-end anastomosis in 2, buccal mucosal graft urethroplasty in 1 and 2-stage repair in 2. Of 14 cases of failure 12 had a satisfactory final outcome, 1 is still waiting for the second stage of urethroplasty and 1 underwent definitive perineostomy. There were 14 patients (23.3%) who experienced ejaculatory dysfunction, 1 (1.6%) a cold glans during erection, 7 (11.6%) a glans that was neither full nor swollen during erection and 11 (18.3%) had decreased glans sensitivity. No patients complained of penile chordee or impotence.
Conclusions: Bulbar end-to-end anastomosis has a success rate of 90.8%. Most patients were satisfied with the surgical outcome despite postoperative complications such as ejaculatory dysfunction, a glans that was neither full nor swollen during erection, or decreased penile sensitivity.
1. Domanda: Per questo tipo di intervento quale tipo di anestesia è previsto?
Risposta: Anestesia generale con intubazione oro-tracheale.
2. Domanda: Quante ore dura l’intervento?
Risposta: Circa due ore.
3. Domanda: Ci sono rischi per l’erezione, la fertilità e la continenza urinaria, dopo l’intervento?
Risposta:No.
4. Domanda: Quanti sono i giorni di degenza in ospedale previsti per questo intervento?
Risposta: In genere il ricovero ospedaliero varia da 5 a 7 giorni.
5. Domanda: Per quanto tempo dovrò portare il catetere dopo l’intervento?
Risposta: Il catetere deve rimanere in sede per quattro settimane dopo l’intervento. Fino a quando non verrà effettuata la prima radiografia di controllo postoperatoria.
6. Domanda: Quali particolari limitazioni sono suggerite durante la convalescenza?
Risposta: Durante la convalescenza è suggerito l’uso di un antibiotico per via orale fino a che non viene rimosso il catetere. È suggerito di non effettuare lungi viaggi in auto, lavori pesanti, attività sessuale e sportiva.
7. Domanda: Quanto tempo dopo l’intervento potrò riprendere la mia attività lavorativa, sportiva e sessuale?
Risposta: Le attività lavorativa, sportiva e sessuale possono essere riprese gradualmente dopo circa 30 giorni dalla rimozione del catetere.
8. Domanda: Dopo l’intervento posso usare la bicicletta od il motorino?
Risposta: L’uso di bicicletta, motorino, cavallo, mezzi a sella in palestra sono sconsigliati.
9. Domanda: Quali cibi e bevande devo evitare dopo l’intervento?
Risposta: L’uso di birra, vini spumanti e gassati sono controindicati. Un uso esagerato di cioccolata, cacao, frutta secca, crostacei non è consigliato.
Tecnica chirurgica: step by step