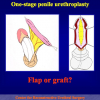
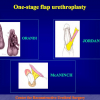
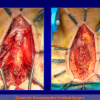
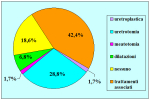
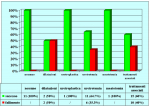
L’intervento denominato “uretroplastica in tempo unico con innesto di cute o mucosa orale” consiste nell’aprire completamente l’uretra nel punto in cui è presente la stenosi ed allargare il canale con un innesto di cute o mucosa orale. Fondamentalmente, esistono tre tipi di uretroplastica peniena in tempo unico:
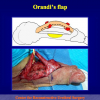
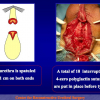
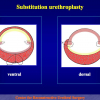
- Uretroplastica in tempo unico con lembo cutaneo. In questa procedura, l’uretra viene allargata con un lembo peduncolizzato di cute penieno (figura 1).
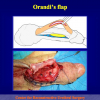
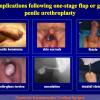
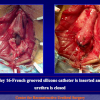
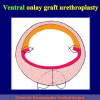
- Uretroplastica in tempo unico con innesto di mucosa orale. In questa procedura, l’uretra viene allargata con un trapianto di mucosa orale (figura 2).
- Uretroplastica in tempo unico con innesto di cute. In questa procedura, l’uretra viene allargata con un trapianto di cute peniena (figura 2).
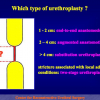
L’intervento chirurgico denominato Uretroplastica con innesto di cute o mucosa orale è indicato fondamentalmente nei seguenti casi:
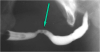
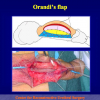
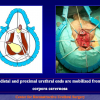
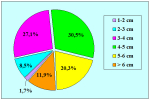
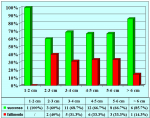
- pazienti con stenosi, non obliterative, dell’uretra peniena di lunghezza superiore a 2 cm (figura 3).
|
Figura 1 |
Figura 2 |
Figura 3 |
Lettura n° 1:
| Which type of urethroplasty – a critical overview of results and complications 22nd Annual EAU Congress March 21-24, 2007 Berlin – Germany |
 scarica PDF |
|
|
|
||
| Lettura n° 2: | ||
| Which type of urethroplasty. A critical overview of results and complications 23rd Annual EAU Congress ESU Course 8 March 26-29, 2008 Milan – Italy |
 scarica PDF scarica PDF |
|
|
|
||
| Lettura n° 3: | ||
| Penile Urethroplasty III Simposio Internacional de Cirurgia Urologica Reconstrutora April 11-12, 2008 Rio de Janeiro-Brazil |
 scarica PDF scarica PDF |
|
|
|
||
| Lettura n° 4: | ||
| Urethral Reconstructive Surgery: Current Trends Portuguese Andrological Association National Meeting June 21 – 23, 2008 Porto – Portugal |
 scarica PDF scarica PDF |
|
|
|
||
| Lettura n° 5: | ||
| Penile and bulbar urethroplasty Surgical techniques and results Hong Kong Urological Association Urethroplasty Workshop Division of Urology – Tuen Mun Hospital Hong Kong February 9 – 10, 2009 |
 scarica PDF scarica PDF |
Articolo n° 1
Barbagli G, Selli C, Tosto A, Palminteri E.
Dorsal free graft urethroplasty.
J Urol. 1996 Jan;155(1):123-6.
Articolo n° 2
Barbagli G, Palminteri E, Lazzeri M.
Dorsal onlay techniques for urethroplasty.
Urol Clin North Am. 2002 May;29(2):389-95.
Articolo n° 3
Barbagli G, Palminteri E, Balò S, Picinotti A, Lazzeri M,
Dorsal onlay graft urethroplasty. Current technique step-by-step.
Contemporary Urology, 2002: 14(5), 18-32
Articolo n° 4
Barbagli G, Palminteri E, Lazzeri M, Guazzoni G.
Anterior urethral strictures.
BJU Int. 2003 Sep;92(5):497-505.
Articolo n° 5
Barbagli G, Palminteri E, Bracka A, Caparros Sariol J.
Penile urethral reconstruction: concepts and concerns.
Arch Esp Urol. 2003 Jun;56(5):549-56.
Articolo n° 6
Barbagli G, Palminteri E, Lazzeri M, Bracka A.
Penile and bulbar urethroplasty using dorsal onlay techniques.
Atlas Urol Clin., 2003: 11, 29-41
Articolo n° 7
Guido Barbagli, Enzo Palminteri, Stefano De Stefani and Massimo Lazzeri
Penile urethroplasty: theniques and outcomes using buccal mucosa grafts.
Contemporary Urology. March 2006, 25-33
1. Domanda: Per questo tipo di intervento quale tipo di anestesia è previsto?
Risposta: Anestesia generale con intubazione nasale.
2. Domanda: Quante ore dura l’intervento?
Risposta: Circa due ore.
3. Domanda: Ci sono rischi per l’erezione, la fertilità e la continenza urinaria, dopo l’intervento?
Risposta: No.
4. Domanda: Quanti sono i giorni di degenza in ospedale previsti per questo intervento?
Risposta: In genere il ricovero ospedaliero varia da 5 a 7 giorni.
5. Domanda: Per quanto tempo dovrò portare il catetere dopo l’intervento? È doloroso portare il catetere?
Risposta: Il catetere deve rimanere in sede per due o tre settimane dopo l’intervento. Il catetere è ben tollerato e non crea particolari problemi in quanto è di piccolo calibro e di puro silicone.
6. Domanda: Quali particolari limitazioni sono suggerite durante la convalescenza?
Risposta: Durante la convalescenza è suggerito l’uso di un antibiotico per via orale fino a che non viene rimosso il catetere. È suggerito di non effettuare lungi viaggi in auto, lavori pesanti, attività sessuale e sportiva.
7. Domanda: Quanto tempo dopo l’intervento potrò riprendere la mia attività lavorativa, sportiva e sessuale?
Risposta: Le attività lavorativa, sportiva e sessuale possono essere riprese gradualmente dopo circa 30 giorni dalla rimozione del catetere.
8. Domanda: Dopo l’intervento posso usare la bicicletta od il motorino?
Risposta: Si.
9. Domanda: Quali cibi e bevande devo evitare dopo l’intervento?
Risposta: L’uso di birra, vini spumanti e gassati sono controindicati. Un uso esagerato di cioccolata, cacao, frutta secca, crostacei non è consigliato.
Risposta: Anestesia generale con intubazione nasale.
2. Domanda: Quante ore dura l’intervento?
Risposta: Circa due ore.
3. Domanda: Ci sono rischi per l’erezione, la fertilità e la continenza urinaria, dopo l’intervento?
Risposta: No.
4. Domanda: Quanti sono i giorni di degenza in ospedale previsti per questo intervento?
Risposta: In genere il ricovero ospedaliero varia da 5 a 7 giorni.
5. Domanda: Per quanto tempo dovrò portare il catetere dopo l’intervento? È doloroso portare il catetere?
Risposta: Il catetere deve rimanere in sede per due o tre settimane dopo l’intervento. Il catetere è ben tollerato e non crea particolari problemi in quanto è di piccolo calibro e di puro silicone.
6. Domanda: Quali particolari limitazioni sono suggerite durante la convalescenza?
Risposta: Durante la convalescenza è suggerito l’uso di un antibiotico per via orale fino a che non viene rimosso il catetere. È suggerito di non effettuare lungi viaggi in auto, lavori pesanti, attività sessuale e sportiva.
7. Domanda: Quanto tempo dopo l’intervento potrò riprendere la mia attività lavorativa, sportiva e sessuale?
Risposta: Le attività lavorativa, sportiva e sessuale possono essere riprese gradualmente dopo circa 30 giorni dalla rimozione del catetere.
8. Domanda: Dopo l’intervento posso usare la bicicletta od il motorino?
Risposta: Si.
9. Domanda: Quali cibi e bevande devo evitare dopo l’intervento?
Risposta: L’uso di birra, vini spumanti e gassati sono controindicati. Un uso esagerato di cioccolata, cacao, frutta secca, crostacei non è consigliato.
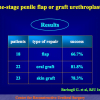
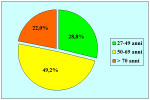
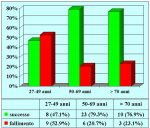
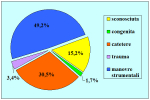
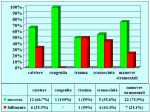
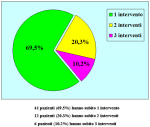
| Risultati aggiornati al 31 dicembre 2021 | |||

Tabella pazienti |
|||
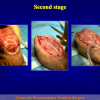
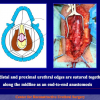
Tecnica chirurgica: step by step
 scarica PDF |