L’intervento denominato “uretroplastica con innesto di mucosa orale” consiste nell’aprire completamente l’uretra nel punto in cui è presente la stenosi ed allargare il canale con un innesto di mucosa orale.
|
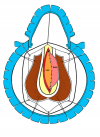
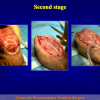
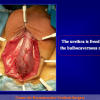
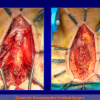
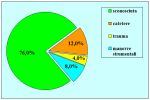
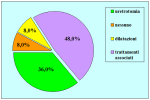
Figura 1 |
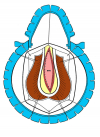
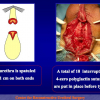
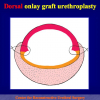
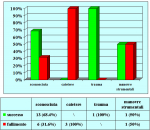
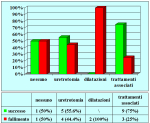
Figura 2 |
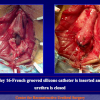
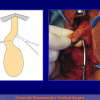
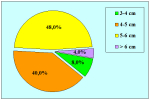
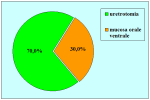
Figura 3 |
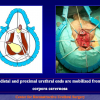
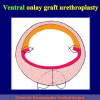
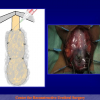
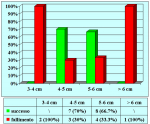
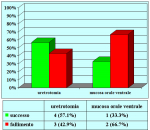
Figura 4 |
Fondamentalmente, esistono quattro tipi di uretroplastica con innesto di mucosa orale:
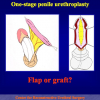
- Uretroplastica con innesto ventrale di mucosa orale. In questa procedura, la mucosa orale viene suturata nella faccia ventrale del canale uretrale (figure 1,2).
- Uretroplastica con innesto dorsale di cute o mucosa orale. In questa procedura, la cute o la mucosa orale vengono suturate nella faccia dorsale del canale uretrale (figure 3,4).
- Uretroplastica con innesto laterale di mucosa orale. In questa procedura, la mucosa orale viene suturata nella faccia laterale del canale uretrale.
- Uretroplastica con sostituzione completa di mucosa orale. In questa procedura, la mucosa uretrale viene sostituita completamente con la mucosa orale.
L’intervento chirurgico denominato Uretroplastica con innesto di cute o mucosa orale è indicato fondamentalmente nei pazienti con stenosi, non traumatica, dell’uretra bulbare di lunghezza superiore a 2 cm.
Lettura n° 1:
| Penile and bulbar urethroplasty Surgical techniques and results Hong Kong Urological Association Urethroplasty Workshop Division of Urology – Tuen Mun Hospital February 9 – 10, 2009 Hong Kong |
 scarica PDF |
Articolo n° 1
Barbagli G, Selli C, di Cello V, Mottola A.
A one-stage dorsal free-graft urethroplasty for bulbar urethral strictures.
Br J Urol. 1996 Dec;78(6):929-32
Articolo n° 2
Barbagli G, Selli C, Tosto A, Palminteri E.
Dorsal free graft urethroplasty.
J Urol. 1996 Jan;155(1):123-6.
Articolo n° 3
Barbagli G, Palminteri E, Rizzo M.
Dorsal onlay graft urethroplasty using penile skin or buccal mucosa in adult bulbourethral strictures.
J Urol. 1998 Oct;160(4):1307-9.
Articolo n° 4
Palminteri E, Lazzeri M, Guazzoni G, Turini D, Barbagli G.
New 2-stage buccal mucosal graft urethroplasty.
J Urol. 2002 Jan;167(1):130-2.
Articolo n° 5
Barbagli G, Palminteri E, Balò S, Picinotti A, Lazzeri M,
Dorsal onlay graft urethroplasty. Current technique step-by-step.
Contemporary Urology, 2002: 14(5), 18-32
Articolo n° 6
Barbagli G, Palminteri E, Lazzeri M, Bracka A.
Penile and bulbar urethroplasty using dorsal onlay techniques.
Atlas Urol Clin., 2003: 11, 29-41
Articolo n° 7
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Interim outcomes of dorsal skin graft bulbar urethroplasty.
JUrol. Volume 172, Issue 4, Pages 1365-1367 (October 2004)
Articolo n° 8
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Bulbar urethroplasty using buccal mucosa grafts placed on the ventral, dorsal or lateral surface of the urethra: are results affected by the surgical technique?
J Urol. 2005 Sep;174(3):955-7;
Articolo n° 9
Barbagli G, De Stefani S, Sighinolfi MC, Annino F, Micali S, Bianchi G.
Bulbar urethroplasty with dorsal onlay buccal mucosal graft and fibrin glue.
Eur Urol. 2006 Sep;50(3):467-74
Articolo n° 10
Barbagli G, De Stefani S, Sighinolfi MC, Pollastri CA, Annino F, Micali S, Bianchi G.
Experience with fibrin glue in bulbar urethral reconstruction using dorsal buccal mucosa graft.
Urology. 2006 Apr;67(4):830-2.
Articolo n° 11
Guido Barbagli, Giuseppe Morgia, Massimo Lazzeri c
Dorsal Onlay Skin Graft Bulbar Urethroplasty: Long-Term Follow-Up
Eur. Urol. 2008,53:628 – 634
Articolo n° 12
Barbagli G., Guazzoni G., Lazzeri M.,
One-Stage bulbar urethroplasty: Retrospective analisys of the results in 375 patients
Eur Urol 2008; 53:828 – 33
Articolo n° 13
Barbagli G, De Stefani S, Annino F, De Carne C, Bianchi G.,
Muscle- and Nerve-sparing Bulbar Urethroplasty: A New Technique.
Eur Urol 2008; 54:335 – 343
Barbagli G, Selli C, di Cello V, Mottola A.
A one-stage dorsal free-graft urethroplasty for bulbar urethral strictures.
Br J Urol. 1996 Dec;78(6):929-32
Articolo n° 2
Barbagli G, Selli C, Tosto A, Palminteri E.
Dorsal free graft urethroplasty.
J Urol. 1996 Jan;155(1):123-6.
Articolo n° 3
Barbagli G, Palminteri E, Rizzo M.
Dorsal onlay graft urethroplasty using penile skin or buccal mucosa in adult bulbourethral strictures.
J Urol. 1998 Oct;160(4):1307-9.
Articolo n° 4
Palminteri E, Lazzeri M, Guazzoni G, Turini D, Barbagli G.
New 2-stage buccal mucosal graft urethroplasty.
J Urol. 2002 Jan;167(1):130-2.
Articolo n° 5
Barbagli G, Palminteri E, Balò S, Picinotti A, Lazzeri M,
Dorsal onlay graft urethroplasty. Current technique step-by-step.
Contemporary Urology, 2002: 14(5), 18-32
Articolo n° 6
Barbagli G, Palminteri E, Lazzeri M, Bracka A.
Penile and bulbar urethroplasty using dorsal onlay techniques.
Atlas Urol Clin., 2003: 11, 29-41
Articolo n° 7
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Interim outcomes of dorsal skin graft bulbar urethroplasty.
JUrol. Volume 172, Issue 4, Pages 1365-1367 (October 2004)
Articolo n° 8
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Bulbar urethroplasty using buccal mucosa grafts placed on the ventral, dorsal or lateral surface of the urethra: are results affected by the surgical technique?
J Urol. 2005 Sep;174(3):955-7;
Articolo n° 9
Barbagli G, De Stefani S, Sighinolfi MC, Annino F, Micali S, Bianchi G.
Bulbar urethroplasty with dorsal onlay buccal mucosal graft and fibrin glue.
Eur Urol. 2006 Sep;50(3):467-74
Articolo n° 10
Barbagli G, De Stefani S, Sighinolfi MC, Pollastri CA, Annino F, Micali S, Bianchi G.
Experience with fibrin glue in bulbar urethral reconstruction using dorsal buccal mucosa graft.
Urology. 2006 Apr;67(4):830-2.
Articolo n° 11
Guido Barbagli, Giuseppe Morgia, Massimo Lazzeri c
Dorsal Onlay Skin Graft Bulbar Urethroplasty: Long-Term Follow-Up
Eur. Urol. 2008,53:628 – 634
Articolo n° 12
Barbagli G., Guazzoni G., Lazzeri M.,
One-Stage bulbar urethroplasty: Retrospective analisys of the results in 375 patients
Eur Urol 2008; 53:828 – 33
Articolo n° 13
Barbagli G, De Stefani S, Annino F, De Carne C, Bianchi G.,
Muscle- and Nerve-sparing Bulbar Urethroplasty: A New Technique.
Eur Urol 2008; 54:335 – 343
1. Domanda: Per questo tipo di intervento quale tipo di anestesia è previsto?
Risposta: Anestesia generale con intubazione nasale.
2. Domanda: Quante ore dura l’intervento?
Risposta: Circa due ore
3. Domanda: Ci sono rischi per l’erezione, la fertilità e la continenza urinaria, dopo l’intervento?
Risposta: No
4. Domanda: Quanti sono i giorni di degenza in ospedale previsti per questo intervento?
Risposta: In genere il ricovero ospedaliero varia da 5 a 7 giorni.
5. Domanda: Per quanto tempo dovrò portare il catetere dopo l’intervento?
Risposta: Il catetere deve rimanere in sede per quattro settimane dopo l’intervento. Fino a quando non verrà effettuata la prima radiografia di controllo postoperatoria.
6. Domanda: Quali particolari limitazioni sono suggerite durante la convalescenza?
Risposta: Durante la convalescenza è suggerito l’uso di un antibiotico per via orale fino a che non viene rimosso il catetere. È suggerito di non effettuare lungi viaggi in auto, lavori pesanti, attività sessuale e sportiva.
7. Domanda: Quanto tempo dopo l’intervento potrò riprendere la mia attività lavorativa, sportiva e sessuale?
Risposta: Le attività lavorativa, sportiva e sessuale possono essere riprese gradualmente dopo circa 30 giorni dalla rimozione del catetere.
8. Domanda: Dopo l’intervento posso usare la bicicletta od il motorino?
Risposta: L’uso di bicicletta, motorino, cavallo, mezzi a sella in palestra sono sconsigliati.
9. Domanda: Quali cibi e bevande devo evitare dopo l’intervento?
Risposta: L’uso di birra, vini spumanti e gassati sono controindicati. Un uso esagerato di cioccolata, cacao, frutta secca, crostacei non è consigliato.
Risposta: Anestesia generale con intubazione nasale.
2. Domanda: Quante ore dura l’intervento?
Risposta: Circa due ore
3. Domanda: Ci sono rischi per l’erezione, la fertilità e la continenza urinaria, dopo l’intervento?
Risposta: No
4. Domanda: Quanti sono i giorni di degenza in ospedale previsti per questo intervento?
Risposta: In genere il ricovero ospedaliero varia da 5 a 7 giorni.
5. Domanda: Per quanto tempo dovrò portare il catetere dopo l’intervento?
Risposta: Il catetere deve rimanere in sede per quattro settimane dopo l’intervento. Fino a quando non verrà effettuata la prima radiografia di controllo postoperatoria.
6. Domanda: Quali particolari limitazioni sono suggerite durante la convalescenza?
Risposta: Durante la convalescenza è suggerito l’uso di un antibiotico per via orale fino a che non viene rimosso il catetere. È suggerito di non effettuare lungi viaggi in auto, lavori pesanti, attività sessuale e sportiva.
7. Domanda: Quanto tempo dopo l’intervento potrò riprendere la mia attività lavorativa, sportiva e sessuale?
Risposta: Le attività lavorativa, sportiva e sessuale possono essere riprese gradualmente dopo circa 30 giorni dalla rimozione del catetere.
8. Domanda: Dopo l’intervento posso usare la bicicletta od il motorino?
Risposta: L’uso di bicicletta, motorino, cavallo, mezzi a sella in palestra sono sconsigliati.
9. Domanda: Quali cibi e bevande devo evitare dopo l’intervento?
Risposta: L’uso di birra, vini spumanti e gassati sono controindicati. Un uso esagerato di cioccolata, cacao, frutta secca, crostacei non è consigliato.
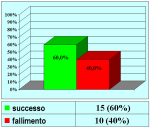
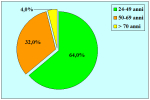
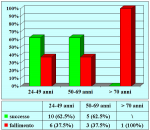
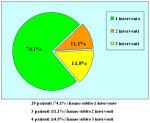
| Risultati aggiornati al 31 dicembre 2021 | |||

Tabella pazienti |
|||
Tecnica chirurgica: step by step
 scarica PDF |