论文 1
Barbagli G, Selli C, di Cello V, Mottola A.
A one-stage dorsal free-graft urethroplasty for bulbar urethral strictures
Br J Urol. 1996 Dec;78(6):929-32
Objective: To report the use of one-stage dorsal free-graft urethroplasty to reduce the incidence of urethrocele.
Patients and Methods: From 1990 to 1994, 20 men (age range 21-86 years) underwent a one-stage dorsal free-graft urethroplasty of bulbar urethral strictures (iatrogenic in 12, traumatic in three, inflammatory in three and unknown in two). All patients except one had been treated previously by optical urethrotomy from one to 14 times.
Results: Temporary fistulae were detected on post-operative urethrography in three patients with particularly long grafts, but they all resolved spontaneously. Within a mean follow-up of 46 months, only one patient had a short recurrent stricture, which was treated successfully by optical urethrotomy. Two patients complained of post-voiding dribbling, but radiographic studies never showed graft weakening and the urinary flow rate was always > 14 mL/s.
Conclusions: Free skin grafts can be applied successfully to the dorsal aspect and by doing so the complications of urethral reconstruction can be reduced.
论文 2
Barbagli G, Palminteri E, Bartoletti R, Selli C, Rizzo M.
Long-term results of anterior and posterior urethroplasty with actuarial evaluation of the success rates.
J Urol. 1997 Oct;158(4):1380-2.
Purpose: We analyzed the long-term results of different urethroplasty techniques.
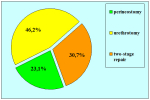
Materials and Methods: We performed a retrospective review of 98 patients who underwent different procedures for anterior (78) and posterior (20) urethral strictures. Mean followup was 53 months. A total of 20 patients underwent end-to-end anastomosis (group 1), 30 underwent 1-stage procedures (group 2), 28 underwent 2-stage procedures (group 3), and 20 underwent bulboprostatic anastomosis (group 4). The results were analyzed using Kaplan-Meier curves and log rank test.
Results: The success rate was 95% for group 1, 93.4% for group 2, 78.6% for group 3, and 70% for group 4. Statistical evaluation of the actuarial success rates failed to show significant differences among the 4 groups.
Conclusions: The stricture recurrences were uniformly distributed over time. Urethroplasty patients must be followed for the rest of their lives.
论文 3
Barbagli G, Selli C, Tosto A, Palminteri E.
Dorsal free graft urethroplasty
J Urol. 1996 Jan;155(1):123-6
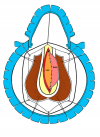
Purpose: Dorsal free graft urethroplasty was performed to reduce the incidence of urethrocele.
Materials and Methods: We treated 12 patients with penile and 13 with bulbous strictures. Of the 13 patients with a bulbous stricture 6 received a dorsally placed tube graft and 7 received a patch graft.
Results: Temporary fistulas were seen on postoperative urethrography in 5 cases but they all resolved spontaneously. At a mean followup of 35.8 months clinical and radiological findings were excellent in 23 cases and good in 2. No signs of graft weakening, such as post-void dribbling or diminished ejaculation, were apparent.
Conclusions: The use of free skin grafts for urethral reconstruction is anatomically healthier in the dorsal than in the ventral position.
论文 4
Barbagli G, Palminteri E, Rizzo M.
Dorsal onlay graft urethroplasty using penile skin or buccal mucosa in adult bulbourethral strictures.
J Urol. 1998 Oct;160(4):1307-9
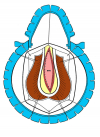
Purpose: Preputial skin graft is used routinely for urethral reconstruction in patients with stricture disease. Alternative donor sites include extrapenile skin, bladder mucosa and buccal mucosa. Recently buccal mucosa graft has been suggested when local epithelial tissue is not available. We describe our experience with 37 patients undergoing 1-stage correction of bulbar urethral stricture using a penile skin (31) or buccal mucosa (6) graft.
Materials and Methods: In 37 patients with bulbar urethral strictures a nontubularized dorsal onlay graft was used for urethral reconstruction. A preputial skin graft was used in 31 patients and a buccal mucosa graft in 6 with a paucity of local skin. Buccal mucosa graft length ranged from 2.5 to 5 cm. (average 4) and preputial skin graft was 2.5 to 12 cm. long (average 4.7). A dorsal approach to the urethral lumen was used in all patients who underwent onlay graft urethroplasty.
Results: Mean followup was 21.5 months for all 37 patients, 23 months for 31 treated with preputial skin graft and 13.5 months for 6 treated with buccal mucosa graft. The clinical outcomes were considered a failure anytime postoperative instrumentation was needed, including dilatation. In the series 34 cases (92%) were classified as a success and 3 (8%) as failure.
Conclusions: Onlay graft urethroplasty provided excellent results in 92% of adults with bulbourethral stricture. The dorsal approach to the urethra allowed the use of foreskin or buccal mucosa graft for reconstruction of the adequate urethral lumen.
论文 5
Barbagli G, Palminteri E, Lazzeri M, Guazzoni G, Turini D.
Long-term outcome of urethroplasty after failed urethrotomy versus primary repair
J Urol. 2001 Jun;165(6 Pt 1):1918-9
Purpose: A urethral stricture recurring after repeat urethrotomy challenges even a skilled urologist. To address the question of whether to repeat urethrotomy or perform open reconstructive surgery, we retrospectively review a series of 93 patients comparing those who underwent primary repair versus those who had undergone urethrotomy and underwent secondary treatment.
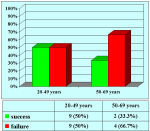
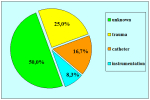
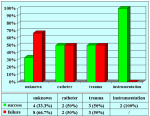
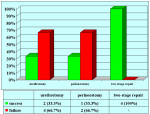
Materials and Methods: From 1975 to 1998, 93 males between age 13 and 78 years (mean 39) underwent surgical treatment for bulbar urethral stricture. In 46 (49%) of the patients urethroplasty was performed as primary repair, and in 47 (51%) after previously failed urethrotomy. The strictures were localized in the bulbous urethra without involvement of penile or membranous tracts. The etiology was ischemic in 37 patients, traumatic in 23, unknown in 17 and inflammatory in 16. To simplify evaluation of the results, the clinical outcome was considered either a success or a failure at the time any postoperative procedure was needed, including dilation.
Results: In our 93 patients primary urethroplasty had a final success rate of 85%, and after failed urethrotomy 87%. Previously failed urethrotomy did not influence the long-term outcome of urethroplasty. The long-term results of different urethroplasty techniques had a final success rate ranging from 77% to 96%.
Conclusions: We conclude that failed urethrotomy does not condition the long-term result of surgical repair. With extended followup, the success rate of urethroplasty decreases with time but it is in fact still higher than that of urethrotomy.
论文 6
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Interim outcomes of dorsal skin graft bulbar urethroplasty.
JUrol. Volume 172, Issue 4, Pages 1365-1367 (October 2004)
Purpose: We update our interim results of bulbar urethroplasty using a skin graft placed on the dorsal urethral surface.
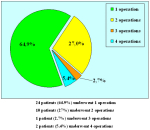
Materials and Methods: A total of 45 patients with an average age of 45 years underwent dorsal onlay skin graft urethroplasty between January 1994 and December 2000. Of the patients 23 had undergone an average of 2.6 prior endoscopic procedures (range 1 to 14). Preoperative evaluation include clinical history, physical examination, retrograde and voiding urethrography, and ultrasonography. In all patients the bulbar urethra was opened along its dorsal surface, the graft was sutured, splayed and quilted to the corpora cavernosa, and the urethra was rotated to cover the graft. In all patients was used penile skin as substitution material. Mean graft length was 4.7 cm (range 2.5 to 11). Three weeks after surgery voiding cystourethrography was performed.
Results: Average follow-up was 71 months (range 41 to 110). Clinical outcome was considered a failure when postoperative instrumentation was needed, including dilation. Of 45 cases 33 (73%) were classified as successful and 12 (27%) were failures. The 12 failures were treated with internal urethrotomy (1), end-to-end-anastomosis (1), skin graft urethroplasty (2) and 2-stage urethroplasty (6). Six of the 12 initial failures had a satisfactory final outcome. The remaining 6 patients refused further surgical procedures and received a definitive perineal urethrostomy.
Conclusion: Penile skin grafts used as a dorsal onlay for bulbar urethral reconstruction in a homogeneous series of patients showed a tendency to deteriorate with time. Longer follow-up is required to compare penile skin with buccal mucosa as substitute materials for bulbar urethral reconstruction.
论文 7
Guido Barbagli, Giuseppe Morgia, Massimo Lazzeri
Dorsal Onlay Skin Graft Bulbar Urethroplasty: Long-Term Follow-Up
Eur. Urol. 2008,53:628 – 634
Objectives: To report retrospectively long-term follow-up in a homogeneous group of patients who underwent dorsal onlay skin graft bulbar urethroplasty and to investigate which factors might influence longterm outcome.
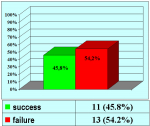
Methods: Thirty-eight patients, with an average age of 43 yr, underwent dorsal onlay skin graft (#12 ventral penile skin and #26 preputial mucosa) bulbar urethroplasty from 1994 to 2000. Of 38 patients, 23 (60.5%) had undergone prior endoscopic procedures. Preoperative evaluation included clinical history, physical examination, retrograde and voiding urethrography, and urethral sonography. Three weeks after surgery, voiding cystourethrography was performed. Patients were followed-up with a clinical evaluation and specific diagnostic tests every 4 mo in the first year and every 12 mo thereafter. Clinical outcome was considered a failure when postoperative instrumentation, including dilation, was needed.
Results: Average follow-up was 111 mo (range, 80–149). Of 38 cases, 25 (65.8%) were successful and 13 (34.2%) failures. Patients with stricture length > 6 cm and a previous history of urethrotomies or dilatations seemed to have a higher risk of failure, but this observation was only a trend and did not reach levels of statistical significance.
Conclusions: Penile skin used as dorsal onlay graft for bulbar urethral reconstruction in a homogeneous series of patients showed a success rate ranging from 90% at short-term follow-up to 66% after long-term follow-up. There was no evidence for particular risk factors (length of stricture, number of dilatations and urethrotomies) for failure.
论文 8
Barbagli G, De Stefani S, Annino F, De Carne C, Bianchi G.
Muscle- and Nerve-sparing Bulbar Urethroplasty: A New Technique.
Eur Urol 2008; 54:335 – 343
Background: To describe a new surgical technique for the repair of bulbar urethral strictures to preserve the bulbospongiosum muscle and its perineal innervation.
Objective: Surgical steps of muscle- and nerve-sparing bulbar urethroplasty are described. The outcome is provided regarding semen sequestration and postvoiding dribbling.
Design, Setting and Participants: We performed the procedure in 12 patients (average age: 43.58 yr) with bulbar urethral strictures (average stricture length: 4.47cm).
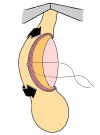
Surgical Procedure: Six patients underwent urethroplasty using a ventral oral mucosal onlay graft, and six patients underwent urethroplasty using a dorsal oral mucosal onlay graft. In all patients, the surgical approach to the bulbar urethra was made avoiding dissection of the bulbospongiosum muscle from the corpus spongiosum and leaving the central tendon of the perineum intact.
Measurements: Clinical outcome was considered a failure when any postoperative instrumentation was needed. The primary outcome examined the technical feasibility of the muscle- and nerve-sparing bulbar urethroplasty. The secondary outcome examined the presence or absence of postoperative postvoid dribbling and semen sequestration using a nonvalidated questionnaire (Appendix).
Results and Limitations: In all patients, postoperative voiding cystourethrography was performed 3 wk after surgery and no urethral sacculation was evident. Urethrography were repeated after 6 mo and 12 mo. No postvoid dribbling or semen sequestration was demonstrated in all patients at 6 mo and 12 mo after surgery. No patient showed stricture recurrence. The average follow-up was 15.25 mo (range 12 mo to 26 mo, median 13.5 mo).
Conclusions: Bulbar urethroplasty preserving the bulbospongiosum muscle, the central tendon of the perineum, and the perineal nerves is a safe, feasible, minimally invasive alternative to traditional bulbar urethroplasty.