论文 1
Barbagli G, Palminteri E, Rizzo M.
Dorsal onlay graft urethroplasty using penile skin or buccal mucosa in adult bulbourethral strictures.
J Urol. 1998 Oct;160(4):1307-9
Purpose: Preputial skin graft is used routinely for urethral reconstruction in patients with stricture disease. Alternative donor sites include extrapenile skin, bladder mucosa and buccal mucosa. Recently buccal mucosa graft has been suggested when local epithelial tissue is not available. We describe our experience with 37 patients undergoing 1-stage correction of bulbar urethral stricture using a penile skin (31) or buccal mucosa (6) graft.
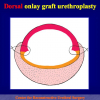
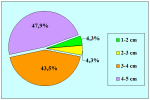
Materials and Methods: In 37 patients with bulbar urethral strictures a nontubularized dorsal onlay graft was used for urethral reconstruction. A preputial skin graft was used in 31 patients and a buccal mucosa graft in 6 with a paucity of local skin. Buccal mucosa graft length ranged from 2.5 to 5 cm. (average 4) and preputial skin graft was 2.5 to 12 cm. long (average 4.7). A dorsal approach to the urethral lumen was used in all patients who underwent onlay graft urethroplasty.
Results: Mean followup was 21.5 months for all 37 patients, 23 months for 31 treated with preputial skin graft and 13.5 months for 6 treated with buccal mucosa graft. The clinical outcomes were considered a failure anytime postoperative instrumentation was needed, including dilatation. In the series 34 cases (92%) were classified as a success and 3 (8%) as failure.
Conclusions: Onlay graft urethroplasty provided excellent results in 92% of adults with bulbourethral stricture. The dorsal approach to the urethra allowed the use of foreskin or buccal mucosa graft for reconstruction of the adequate urethral lumen.
论文 2
Barbagli G, Palminteri E, Lazzeri M.
Dorsal onlay techniques for urethroplasty
Urol Clin North Am. 2002 May;29(2):389-95
Objective: To review the outcome of bulbar urethroplasty using one-stage surgical techniques.
Dorsal onlay graft urethroplasty is a versatile procedure which may be combined with various substitute materials such as preputial skin, buccal mucosa grafts or pedicled flaps. Others substitute materials such as human urethral mucosa from corpses or collagen matrix will be possible in future. The long-term results of a wide series of patients showed a final success rate from 92% to 97%. Any kind of substitution urethroplasty deteriorate over time, and in our series of patients with an extended follow-up from 21.5 to 43 months the success rate of dorsal onlay graft urethroplasty decreased from 92% to 85%. With regard to substitute material concerns (buccal mucosa versus preputial skin) a long-term follow-up is mandatory to establish if buccal mucosa is superior to foreskin as urethral substitute material. At present, the authors currently use both according to patient preference, status of the genital tissues or strictures characteristics.
论文 3
Barbagli G, Palminteri E, Balò S, Picinotti A, Lazzeri M.
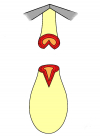
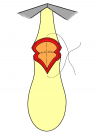
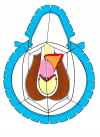
Dorsal onlay graft urethroplasty. Current technique step-by-step.
Contemporary Urology, 2002: 14(5), 18-32
The ideal surgical procedure for long bulbourethral strictures would be simple, reliable, effective over the long term, and reproducible in the hands of any surgeon. The Barbagli procedure – based on sound atomic, historic, and surgical principles – fulfils these criteria.
论文 4
Barbagli G, Palminteri E, Lazzeri M, Guazzoni G.
Anterior urethral strictures.
BJU Int. 2003 Sep;92(5):497-505.
The surgical treatment of adult anterior urethral strictures has developed continuously. Recently considerable changes have been introduced, involving the cause of the urethral disease and surgical techniques. The criteria for selecting the reconstructive surgical technique are presented according to the cause and a new classification of urethral strictures. The main surgical procedures are presented and fully illustrated, with an updated and comprehensive review of recent publications.
论文 5
Barbagli G, Palminteri E, Lazzeri M, Bracka A.
Penile and bulbar urethroplasty using dorsal onlay techniques.
Atlas Urol Clin., 2003: 11, 29-41
The surgical treatment of adult anterior urethral strictures has been a constantly evolving process. Recently, considerable changes have been introduced: the wider use of the buccal mucosa graft and the use of the dorsal onlay approach, also named the Barbagli procedure. Moreover, in penile urethra, the dorsal placement of the graft is now combined by the incision of the urethral plate, as suggested by Snodgrass for childhood hypospadias surgery and its augmentation, as suggested by Bracka, Asopa and Hayes.
Three different techniques are presented:
Penile one-stage urethroplasty with urethral plate incision and augmentation using a dorsal buccal mucosa graft;
Bulbar one-stage urethroplasty with urethral plate augmentation using a dorsal buccal mucosa graft;
Bulbar one-stage urethroplasty with urethral place replacement using a dorsal buccal mucosa graft.
论文 6
Barbagli G, Palminteri E, Guazzoni G, Montorsi F, Turini D, Lazzeri M.
Bulbar urethroplasty using buccal mucosa grafts placed on the ventral, dorsal or lateral surface of the urethra: are results affected by the surgical technique?
J Urol. 2005 Sep;174(3):955-7
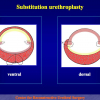
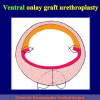
Purpose: The use of buccal mucosa graft onlay urethroplasty represents the most widespread method of bulbar urethral stricture repair. The graft may be placed on the ventral or dorsal urethral surface according to surgeon experience and preference. We investigated whether the results are affected by the surgical technique by comparing the outcome of 3 types of bulbar urethroplasty using buccal mucosa graft.
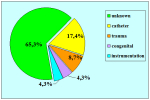
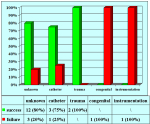
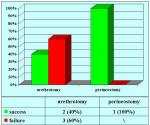
Materials and Methods: We repaired 50 bulbar urethral strictures with buccal mucosa grafts from 1997 to 2002. Mean patient age was 42 years. The etiology of stricture was ischemia in 12 cases, trauma in 6, instrumentation in 4 and unknown in 28. Patients with lichen sclerosus, failed hypospadias or urethroplasty and stricture extending into the penile urethra were not included. A total of 47 patients (94%) had undergone previous urethrotomy or dilation. The buccal mucosa graft was always harvested from the cheek using a 2 team approach. Mean graft length was 4.2 cm. The graft was placed on the ventral, dorsal and lateral bulbar urethral surface in 17, 27 and 6 cases, respectively. Clinical outcome was considered a success or failure at the time that any postoperative procedure was needed, including dilation. Mean followup was 42 months (range 12 to 76).
Results: Of 50 cases 42 (84%) were successful and 8 (16%) failed. The 17 ventral grafts provided success in 14 cases (83%) and failure in 3 (17%). The 27 dorsal grafts provided success in 23 cases (85%) and failure in 4 (15%). The 6 lateral grafts provided success in 5 cases (83%) and failure in 1 (17%). No surgical complications were observed. Failures involved the anastomotic site (distal in 2 and proximal in 3) and the whole grafted area in 3 cases. They were treated with urethrotomy in 5 cases and 2-stage urethroplasty in 3.
Conclusions: In our experience the placement of buccal mucosa grafts into the ventral, dorsal or lateral surface of the bulbar urethra showed the same success rates (83% to 85%) and the outcome was not affected by the surgical technique. Moreover, stricture recurrence was uniformly distributed in all patients.
论文 7
Barbagli G, De Stefani S, Sighinolfi MC, Annino F, Micali S, Bianchi G.
Bulbar urethroplasty with dorsal onlay buccal mucosal graft and fibrin glue.
Eur Urol. 2006 Sep;50(3):467-74. Epub 2006 Jun 5
Objectives: We describe a new surgical technique with the use of fibrin glue for bulbar urethra reconstruction using a dorsal buccal mucosal onlay graft.
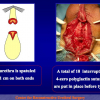
Methods: Six patients with a mean age of 43 yr underwent bulbar urethroplasty with dorsal onlay buccal mucosal graft and fibrin glue. The urethra was mobilised from the corpora cavernosa and opened along its dorsal surface. The buccal mucosal graft was applied on the corpora cavernosa using 2ml of fibrin glue. Two interrupted polyglactin 5-0 sutures were used to fix the apices of the graft to the underlying albuginea of the corpora cavernosa. The urethra was rotated back to cover the graft and an adjunctive fibrin glue was injected over the urethra.
Results: The mean operative time was 100min (range, 90-120min). No intraoperative or postoperative complications were observed. Voiding cystourethrography was performed when the catheter was removed 2 wk after surgery. Urine culture, uroflowmetry, and urethrography were repeated after 6 and 12 mo and annually thereafter. Mean follow-up was 16 mo (range, 12-24 mo). No restrictures at the anastomotic sites were demonstrated in any of the patients 6 and 12 mo after surgery.
Conclusions: The use of fibrin glue represents a slight but significant step toward perfecting the surgical technique of bulbar urethral reconstruction.
论文 8
Barbagli G, De Stefani S, Sighinolfi MC, Pollastri CA, Annino F, Micali S, Bianchi G.
Experience with fibrin glue in bulbar urethral reconstruction using dorsal buccal mucosa graft.
Urology. 2006 Apr;67(4):830-2.
Buccal mucosa dorsal onlay graft urethroplasty represents a widespread method for bulbar urethral stricture repair. We describe a modified procedure with the use of fibrin glue applied on the receiving bed before graft location.
论文9
Barbagli G., Guazzoni G., Lazzeri M.
One-Stage bulbar urethroplasty: Retrospective analisys of the results in 375 patients
Eur Urol 2008; 53:828 – 33
Objective: To review the outcome of bulbar urethroplasty using one-stage surgical techniques.
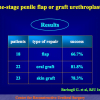
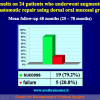
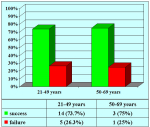
Methods: Of 375 patients, who underwent one-stage bulbar urethroplasties, 165 patients (44%) underwent anastomotic repair (AR), 40 (10.7%) underwent augmented anastomotic repair (AAR) using penile skin grafts (PSGs) or oral mucosal grafts (OMGs), and 170 (45.3%) underwent onlay grafting techniques (OGTs) using PSGs or OMGs. Clinical outcome was considered a failure when any postoperative instrumentation was needed. The chi(2) and Fisher’s exact test for categorical data were used. The sample size of 375 patients provides a statistical power (1-beta) of 99% at alpha=0.05; p<0.05 was set as significant.
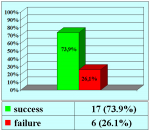
Results: The average follow-up was 53 mo. Of 375 cases, 313 (83.5%) were successful and 62 (16.5%) failures. Of 165 ARs, 150 (90.9%) were successful and 15 (9.1%) failures. Of 40 AARs, 24 (60%) were successful and 16 (40%) failures. Of 170 OGTs, 139 (81.8%) were successful and 31 (18.2%) failures. The AR showed statistically significant higher success rate compared to OGT (p=0.023) and AAR (p=0.0001). Of 47 PSGs, 28 (59.6%) were successful and 19 (40.4%) failures. Of 163 OMGs, 135 (82.8%) were successful and 28 (17.2%) failures. This difference was statistically significant (p=0.002).
Conclusions: One-stage bulbar urethroplasties showed an overall 83.5% success rate. The AR showed the higher success rate compared to the OGT or AAR. OMGs (82.8% success rate) perform statistically better than PSGs (59.6% success rate).
论文 10
Barbagli G, De Stefani S, Annino F, De Carne C, Bianchi G.
Muscle- and Nerve-sparing Bulbar Urethroplasty: A New Technique.
Eur Urol 2008; 54:335 – 343
Background: To describe a new surgical technique for the repair of bulbar urethral strictures to preserve the bulbospongiosum muscle and its perineal innervation.
Objective: Surgical steps of muscle- and nerve-sparing bulbar urethroplasty are described. The outcome is provided regarding semen sequestration and postvoiding dribbling.
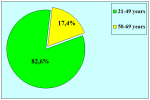
Design, Setting and Participants: We performed the procedure in 12 patients (average age: 43.58 yr) with bulbar urethral strictures (average stricture length: 4.47cm).
Surgical Procedures: Six patients underwent urethroplasty using a ventral oral mucosal onlay graft, and six patients underwent urethroplasty using a dorsal oral mucosal onlay graft. In all patients, the surgical approach to the bulbar urethra was made avoiding dissection of the bulbospongiosum muscle from the corpus spongiosum and leaving the central tendon of the perineum intact.
Measurements: Clinical outcome was considered a failure when any postoperative instrumentation was needed. The primary outcome examined the technical feasibility of the muscle- and nerve-sparing bulbar urethroplasty. The secondary outcome examined the presence or absence of postoperative postvoid dribbling and semen sequestration using a nonvalidated questionnaire (Appendix).
Results and Limitations: In all patients, postoperative voiding cystourethrography was performed 3 wk after surgery and no urethral sacculation was evident. Urethrography were repeated after 6 mo and 12 mo. No postvoid dribbling or semen sequestration was demonstrated in all patients at 6 mo and 12 mo after surgery. No patient showed stricture recurrence. The average follow-up was 15.25 mo (range 12 mo to 26 mo, median 13.5 mo).
Conclusions: Bulbar urethroplasty preserving the bulbospongiosum muscle, the central tendon of the perineum, and the perineal nerves is a safe, feasible, minimally invasive alternative to traditional bulbar urethroplasty.