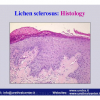
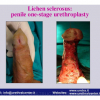
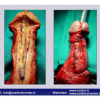
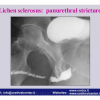
硬化性苔藓会导致疤痕形成,进而造成尿路和性功能障碍,生活质量下降。症状包括瘙痒和烧灼感,包皮上翻困难,尿流细速。体检发现典型的扁平、萎缩的白色或象牙色的融合成不同大小的斑块,经常伴有包皮上翻困难和尿道口狭窄。
 |
 |
 |
 |
讲座 1:
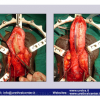
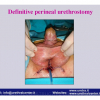
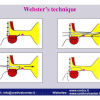
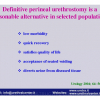
| Reconstruction of urethral strictures due to lichen sclerosus 28th Congress of the Société Internationale d’Urologie November 12 – 16, 2006 Cape Town – South Africa |
 Download PDF |
|
|
|
||
| 讲座 2: | ||
| BXO – Lichen sclerosus III° Simposio Internacional de Cirurgia Urologica Reconstrutora April 11-12, 2008 Rio de Janeiro-Brazil |
 Download PDF |
|
|
|
||
| 讲座 3: | ||
| Lichen sclerosus genito-urinario Società Italiana Urologia Territoriale (SIUT) Urologi Ospedalità Privata (Ur.O.P.) September 22 – 28, 2008 Rome – Italy |
 Download PDF |
|
|
|
||
| 讲座 4: | ||
| Lichen sclerosus Overview: etiology, clinical presentation and management Muljibhai Patel Urological Hospital “URETHROPLASTY” July 19 – 20, 2012 Nadiad – Gujarat – India |
 Download PDF |
论文 1
Lichen sclerosis of male genitalia involving anterior urethra
Lancet 1999; 354(number 9176): 429.
论文 2
Lichen sclerosus involving anterior urethra
J. Urol 1999; 16 1: 102 (Abstract 384).
论文 3
Lichen Sclerosus of the male genitalia
Contemporary Urology 2001; 13:, 47-58.
论文 4
Lichen sclerosus of the male genitalia and urethral stricture diseases
Urol Int 2004; 73: 1-5.
论文 5
Penile carcinoma in patients with genital lichen sclerosus: a multicenter survey
J Urol 2006; 175: 1359-1363.
论文 6
Resurfacing and reconstruction of the glans penis
Eur Urol 2007; 52: 893-900.
论文 7
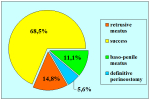
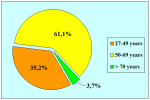
Lichen Sclerosus of the Male Genitalia and Urethra: Surgical Options and Results in a Multicenter International Experience with 215 Patients
Eur Urol 2009; 55: 945-956.
Lichen sclerosis of male genitalia involving anterior urethra
Lancet 1999; 354(number 9176): 429.
论文 2
Lichen sclerosus involving anterior urethra
J. Urol 1999; 16 1: 102 (Abstract 384).
论文 3
Lichen Sclerosus of the male genitalia
Contemporary Urology 2001; 13:, 47-58.
论文 4
Lichen sclerosus of the male genitalia and urethral stricture diseases
Urol Int 2004; 73: 1-5.
论文 5
Penile carcinoma in patients with genital lichen sclerosus: a multicenter survey
J Urol 2006; 175: 1359-1363.
论文 6
Resurfacing and reconstruction of the glans penis
Eur Urol 2007; 52: 893-900.
论文 7
Lichen Sclerosus of the Male Genitalia and Urethra: Surgical Options and Results in a Multicenter International Experience with 215 Patients
Eur Urol 2009; 55: 945-956.
1. 问: 此项手术使用什么麻醉方式?
答: 经鼻或口-气管插管的全身麻醉。
2. 问: 手术时间多长?
答: 大约2小时。
3.问: 手术后是否有勃起功能障碍的风险?
答: 没有。
4. 问: 手术后住院时间是多长?
答: 一般来说,3到5天。
5. 问: 术后多长时间可以拔除尿管?使用尿管是不是很痛?
答: 术后尿管要保留一至两周。尿管管径很小,可以耐受。
6. 问: 恢复期有什么特别需要注意的问题么?
答: 在恢复期,抗生素的使用一般持续到尿管拔除以后。同时,长途坐车旅行,重体力劳动、性生活以及运动是暂时需要避免的。
7. 问: 术后什么时候可以恢复工作、性生活以及运动?
答: 在拔除尿管之后,根据情况逐步恢复即可。
8. 问: 手术以后是否可以立即骑自行车或摩托车?
答: 是的。
9. 问: 术后饮食需要注意些什么?
答: 避免啤酒以及烈性酒精饮品,巧克力,可可,坚果和贝类不要多吃。
答: 经鼻或口-气管插管的全身麻醉。
2. 问: 手术时间多长?
答: 大约2小时。
3.问: 手术后是否有勃起功能障碍的风险?
答: 没有。
4. 问: 手术后住院时间是多长?
答: 一般来说,3到5天。
5. 问: 术后多长时间可以拔除尿管?使用尿管是不是很痛?
答: 术后尿管要保留一至两周。尿管管径很小,可以耐受。
6. 问: 恢复期有什么特别需要注意的问题么?
答: 在恢复期,抗生素的使用一般持续到尿管拔除以后。同时,长途坐车旅行,重体力劳动、性生活以及运动是暂时需要避免的。
7. 问: 术后什么时候可以恢复工作、性生活以及运动?
答: 在拔除尿管之后,根据情况逐步恢复即可。
8. 问: 手术以后是否可以立即骑自行车或摩托车?
答: 是的。
9. 问: 术后饮食需要注意些什么?
答: 避免啤酒以及烈性酒精饮品,巧克力,可可,坚果和贝类不要多吃。
| Up-to-date to 12-31-2021 | |||

总结表 |
|||