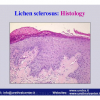
Lichen sclerosus cause destructive scarring that can lead to urinary and sexual problems and a decrease of quality of life. Symptoms are pruritus and soreness, difficulty in retracting the foreskin and a poor urinary stream. Examination shows typical flat, atrophic, ivory to white colored papules that coalesce in plaques of varying sizes, commonly with a non-retractile prepuce and meatal stenosis.
 |
 |
 |
 |
Lecture n° 1:
| Reconstruction of urethral strictures due to lichen sclerosus 28th Congress of the Société Internationale d’Urologie November 12 – 16, 2006 Cape Town – South Africa |
 Download PDF |
|
|
|
||
| Lecture n° 2: | ||
| BXO – Lichen sclerosus III° Simposio Internacional de Cirurgia Urologica Reconstrutora April 11-12, 2008 Rio de Janeiro-Brazil |
 Download PDF |
|
|
|
||
| Lecture n° 3: | ||
| Lichen sclerosus genito-urinario Società Italiana Urologia Territoriale (SIUT) Urologi Ospedalità Privata (Ur.O.P.) September 22 — 28, 2008 Rome – Italy |
 Download PDF |
|
|
|
||
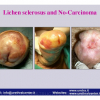
| Lecture n° 4: | ||
| Lichen sclerosus Overview: etiology, clinical presentation and management Muljibhai Patel Urological Hospital «URETHROPLASTY» July 19 – 20, 2012 Nadiad – Gujarat — India |
 Download PDF |
Article n° 1
Lichen sclerosis of male genitalia involving anterior urethra
Lancet 1999; 354(number 9176): 429.
Article n° 2
Lichen sclerosus involving anterior urethra
J. Urol 1999; 16 1: 102 (Abstract 384).
Article n° 3
Lichen Sclerosus of the male genitalia
Contemporary Urology 2001; 13:, 47-58.
Article n° 4
Lichen sclerosus of the male genitalia and urethral stricture diseases
Urol Int 2004; 73: 1-5.
Article n° 5
Penile carcinoma in patients with genital lichen sclerosus: a multicenter survey
J Urol 2006; 175: 1359-1363.
Article n° 6
Resurfacing and reconstruction of the glans penis
Eur Urol 2007; 52: 893-900.
Article n° 7
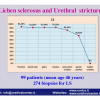
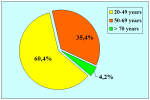
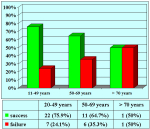
Lichen Sclerosus of the Male Genitalia and Urethra: Surgical Options and Results in a Multicenter International Experience with 215 Patients
Eur Urol 2009; 55: 945-956.
Lichen sclerosis of male genitalia involving anterior urethra
Lancet 1999; 354(number 9176): 429.
Article n° 2
Lichen sclerosus involving anterior urethra
J. Urol 1999; 16 1: 102 (Abstract 384).
Article n° 3
Lichen Sclerosus of the male genitalia
Contemporary Urology 2001; 13:, 47-58.
Article n° 4
Lichen sclerosus of the male genitalia and urethral stricture diseases
Urol Int 2004; 73: 1-5.
Article n° 5
Penile carcinoma in patients with genital lichen sclerosus: a multicenter survey
J Urol 2006; 175: 1359-1363.
Article n° 6
Resurfacing and reconstruction of the glans penis
Eur Urol 2007; 52: 893-900.
Article n° 7
Lichen Sclerosus of the Male Genitalia and Urethra: Surgical Options and Results in a Multicenter International Experience with 215 Patients
Eur Urol 2009; 55: 945-956.
1. Question: What kind of anesthesia is used for this surgery?
Answer: General anesthesia without oro-tracheal intubationt.
2. Question: How many hours does the surgery take?
Answer: About 1/2 hour.
3. Question: Are there any risks concerning erection after the surgery?
Answer: No, there aren’t.
4. Question: How many days of hospital recovery are expected following the surgery?
Answer: In general, from 2 to 3 days.
5. Question: How long will I have to use a catheter after the surgery? Is it painful to use the catheter?
Answer: The catheter must stay in place for 24 hours after the surgery. The catheter is well tolerated because of its small diameter.
6. Question: Are there any particular recommendations during convalescence?
Answer: During convalescence, the use of oral antibiotics is suggested for 5 days. Avoiding sexual activity is also suggested.
7. Question: When will I be able to resume working, sexual activity and sports?
Answer: Work and sports can be resumed immediately. Sexual activity can be resumed 15 days after surgery.
8. Question: Can I ride a bike or a motorcycle immediately after the surgery?
Answer: Yes.
9. Question: What kinds of foods and drinks should be avoided after the surgery?
Answer: None.
Answer: General anesthesia without oro-tracheal intubationt.
2. Question: How many hours does the surgery take?
Answer: About 1/2 hour.
3. Question: Are there any risks concerning erection after the surgery?
Answer: No, there aren’t.
4. Question: How many days of hospital recovery are expected following the surgery?
Answer: In general, from 2 to 3 days.
5. Question: How long will I have to use a catheter after the surgery? Is it painful to use the catheter?
Answer: The catheter must stay in place for 24 hours after the surgery. The catheter is well tolerated because of its small diameter.
6. Question: Are there any particular recommendations during convalescence?
Answer: During convalescence, the use of oral antibiotics is suggested for 5 days. Avoiding sexual activity is also suggested.
7. Question: When will I be able to resume working, sexual activity and sports?
Answer: Work and sports can be resumed immediately. Sexual activity can be resumed 15 days after surgery.
8. Question: Can I ride a bike or a motorcycle immediately after the surgery?
Answer: Yes.
9. Question: What kinds of foods and drinks should be avoided after the surgery?
Answer: None.
| Up-to-date to 12-31-2021 | |||

Summarizing Table |
|||