Hypospadias is a condition manifested by 3 anatomical problems, including an abnormal site of the urethral meatus, penile curvature and abnormal foreskin development or dorsal hooded foreskin. It is the most common congenital penile anomaly, occurring in 1/300 live births with a multifactorial aetiology of genetic susceptibility plus endocrine disruptors. Recent studies show that the incidence of hypospadias is increasing in Western countries, and even higher incidence is expected in developing countries and in the Third World.
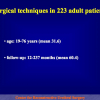
The American Academy of Paediatrics recommends performing hypospadias repair at ages 6 to 12 months. The current standard of care is to repair hypospadias with a 1-stage procedure on an outpatient basis to improve the appearance of the penis, allow voiding while standing, and improve the chances of fertility.
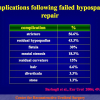
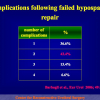
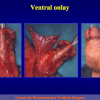
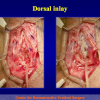
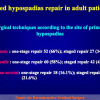
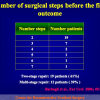
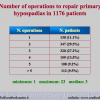
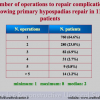
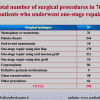
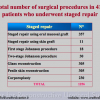
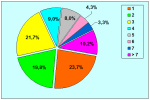
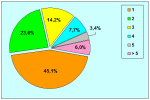
The repair of primary hypospadias may result in postoperative complications requiring secondary surgery, such as fistula, diverticulum, retrusive urethral meatus, residual chordee, and stricture. These operative failures during primary repair are caused by errors in design, technique and postoperative care, such as infection, wound dehiscence, urine extravasation, haematoma, ischemia and necrosis of transplanted tissues. Hypospadias repair may also fail many years after achieving successful functional and cosmetic results by primary repair and urethral strictures may develop decades after the initial hypospadias surgery. Treatment for complications in children and adults with a history of paediatric hypospadias repair remains complex because the penis is densely scarred, immobile, hypovascular or significantly shortened. Epidemiological data on the incidence of failed hypospadias repair and the number of adults seeking further surgical treatment remains unknown. This may by due to the fact that the pediatric followup stops early in the patient lifetime and the urologist takes over late in the lifetime.
Management of complications in patients in whom multiple attempts of hypospadias repair have failed is still a complex problem for the health care system, involving health care providers, general practitioners, pediatricians, surgeons, patients and parents because this difficult population of patients has been left with deformities that are significantly worse than the primary congenital anomaly.
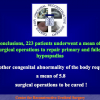
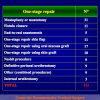
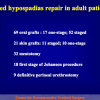
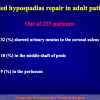
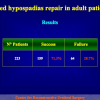
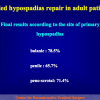
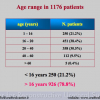
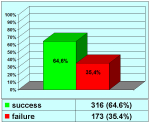
In our Center, 14.7% of 1,510 patients treated for urethral stricture disease, and 51% of patients treated for penile urethral strictures showed failed hypospadias repair. Half of the patients with penile strictures had a history of failed hypospadias. The data probably underestimate the true incidence of this problem in the adult population.
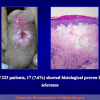
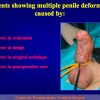
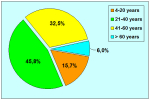
Our experience shows 2 adult populations with failed hypospadias repair. Some patients had multiple penile deformities significantly worse than the primary congenital anomaly, such as fistula, residual hypospadias, penile curvature and cosmetically unacceptable glans or penile skin appearance. On the other hand, some patients had a satisfactory result of primary hypospadias repair with a cosmetically acceptable meatus and no evident penile deformities, but they had obstructive symptoms due to urethral stricture. These patients had increasing urinary problems and difficulties many years after surgery when pediatric followup had already stopped and they were fully involved in sexual activity. In these patients the congenital lack of spongiosum tissue may promote urethral deterioration with time. Probably, the new skin urethra cannot tolerate the repeated stretch and trauma during erection and sexual activity, which is tolerate by the normal normal spongiosum urethra. As an analogy, during sexual activity the corpus spongiosum is to the urethra what the airbag is to the body during a motor vehicle accident.
The American Academy of Paediatrics recommends performing hypospadias repair at ages 6 to 12 months. The current standard of care is to repair hypospadias with a 1-stage procedure on an outpatient basis to improve the appearance of the penis, allow voiding while standing, and improve the chances of fertility.
The repair of primary hypospadias may result in postoperative complications requiring secondary surgery, such as fistula, diverticulum, retrusive urethral meatus, residual chordee, and stricture. These operative failures during primary repair are caused by errors in design, technique and postoperative care, such as infection, wound dehiscence, urine extravasation, haematoma, ischemia and necrosis of transplanted tissues. Hypospadias repair may also fail many years after achieving successful functional and cosmetic results by primary repair and urethral strictures may develop decades after the initial hypospadias surgery. Treatment for complications in children and adults with a history of paediatric hypospadias repair remains complex because the penis is densely scarred, immobile, hypovascular or significantly shortened. Epidemiological data on the incidence of failed hypospadias repair and the number of adults seeking further surgical treatment remains unknown. This may by due to the fact that the pediatric followup stops early in the patient lifetime and the urologist takes over late in the lifetime.
Management of complications in patients in whom multiple attempts of hypospadias repair have failed is still a complex problem for the health care system, involving health care providers, general practitioners, pediatricians, surgeons, patients and parents because this difficult population of patients has been left with deformities that are significantly worse than the primary congenital anomaly.
In our Center, 14.7% of 1,510 patients treated for urethral stricture disease, and 51% of patients treated for penile urethral strictures showed failed hypospadias repair. Half of the patients with penile strictures had a history of failed hypospadias. The data probably underestimate the true incidence of this problem in the adult population.
Our experience shows 2 adult populations with failed hypospadias repair. Some patients had multiple penile deformities significantly worse than the primary congenital anomaly, such as fistula, residual hypospadias, penile curvature and cosmetically unacceptable glans or penile skin appearance. On the other hand, some patients had a satisfactory result of primary hypospadias repair with a cosmetically acceptable meatus and no evident penile deformities, but they had obstructive symptoms due to urethral stricture. These patients had increasing urinary problems and difficulties many years after surgery when pediatric followup had already stopped and they were fully involved in sexual activity. In these patients the congenital lack of spongiosum tissue may promote urethral deterioration with time. Probably, the new skin urethra cannot tolerate the repeated stretch and trauma during erection and sexual activity, which is tolerate by the normal normal spongiosum urethra. As an analogy, during sexual activity the corpus spongiosum is to the urethra what the airbag is to the body during a motor vehicle accident.
Lecture n° 1:
| Failed hypospadias presenting in adults 2006 ESGURS Third Congress September 29 — 30, 2006 Milan — Italy |
 scarica PDF scarica PDF |
|
|
|
||
| Lecture n° 2: | ||
| Failed hypospadias repair presenting in adults International Congress on Hypospadias Surgery September 2-5, 2007 Prishtina – Kosova |
 scarica PDF scarica PDF |
|
|
|
||
| Lecture n° 3: | ||
| Hypospadias: problems in the adult patients 24th Annual EAU Congress March 17-21, 2009 Stockholm – Sweden |
 scarica PDF |
|
|
|
||
| Lecture n° 4: | ||
| Failed Hypospadias Repair 2nd Surgical Workshop of Complex Uro-Genital Reconstructive Surgery in Adulthood September 11-12, 2009 Belgrade — Serbia |
 scarica PDF |
|
| Lecture n° 5: | ||
| Problems of urethral stricture in adult male after penile and urethral reconstructive surgery in childood 41st Scientific Congress September 8 — 10, 2011 Gdańsk – Poland |
 Download PDF |
|
|
|
||
| Lecture n° 6: | ||
| Surgical options in adult patients with failed hypospadias repair 9th Conference of the Arab Association of Urology 7th International Conference of Jordanian Association of Urological Surgeons November 22 — 24, 2011 Amman – Jordan |
 Download PDF |
Article n° 1
Failed hypospadias repair presenting in adults
Eur Urol. 2006 May;49(5):887-94
Article n° 2
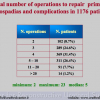
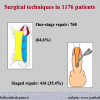
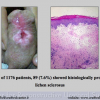
Retrospective Descriptive Analysis of 1,176 Patients With Failed Hypospadias Repair
J Urol 2010; 183: 207-211
Article n° 3
Surgical challenge in patients who underwent failed hypospadias repair: it is time to change?
Urol Int 2010; 85: 427-435
Article n° 4
Surgical Repair of Late Complications in Patients Having Undergone Primary Hypospadias Repair during Childhood: A New Perspective
Hindawi Publishing Corporation
Advances in Urology
Volume 2012, Article ID 705212, 5 pages
Failed hypospadias repair presenting in adults
Eur Urol. 2006 May;49(5):887-94
Article n° 2
Retrospective Descriptive Analysis of 1,176 Patients With Failed Hypospadias Repair
J Urol 2010; 183: 207-211
Article n° 3
Surgical challenge in patients who underwent failed hypospadias repair: it is time to change?
Urol Int 2010; 85: 427-435
Article n° 4
Surgical Repair of Late Complications in Patients Having Undergone Primary Hypospadias Repair during Childhood: A New Perspective
Hindawi Publishing Corporation
Advances in Urology
Volume 2012, Article ID 705212, 5 pages
1. Question: What kind of anesthesia is used for this surgery?
Answer: General anesthesia with nasal or oro-tracheal intubation.
2. Question: How many hours does the surgery take?
Answer: About 2 hour.
3. Question: Are there any risks concerning erection?
Answer: No.
4. Question: How many days of hospital recovery are expected following the surgery?
Answer: In general, from 2 to 4 days.
5. Question: How long will I have to use a urethral catheter following surgery?
Answer: The urethral catheter must stay in place for one or two weeks following surgery.
6. Question: Are there any particular recommendations during convalescence?
Answer: During convalescence, antibiotic use is suggested until the catheter is removed. It is also suggested that sexual activity be avoided.
7. Question: When will I be able to resume sexual activity?
Answer: Sexual activity can be gradually resumed one month after surgery.
8. Question: Can I ride a bike or a motorcycle immediately after the surgery?
Answer: Yes.
9. Question: What kinds of foods and drinks should be avoided after the surgery?
Answer: None.
Answer: General anesthesia with nasal or oro-tracheal intubation.
2. Question: How many hours does the surgery take?
Answer: About 2 hour.
3. Question: Are there any risks concerning erection?
Answer: No.
4. Question: How many days of hospital recovery are expected following the surgery?
Answer: In general, from 2 to 4 days.
5. Question: How long will I have to use a urethral catheter following surgery?
Answer: The urethral catheter must stay in place for one or two weeks following surgery.
6. Question: Are there any particular recommendations during convalescence?
Answer: During convalescence, antibiotic use is suggested until the catheter is removed. It is also suggested that sexual activity be avoided.
7. Question: When will I be able to resume sexual activity?
Answer: Sexual activity can be gradually resumed one month after surgery.
8. Question: Can I ride a bike or a motorcycle immediately after the surgery?
Answer: Yes.
9. Question: What kinds of foods and drinks should be avoided after the surgery?
Answer: None.
| Up-to-date to 12-31-2021 | |||

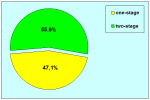
PDF One-stage |

PDF Two-stage |

Summarizing table |
|